Have an even better birth.
Online birth classes and resources to help you feel prepared and in control — no matter how you deliver.

YOU’RE ABOUT TO BIRTH A WHOLE-A** HUMAN
Of course you’re nervous.
As your due date gets closer, so do all those nagging what-ifs:
- What if I can’t handle the pain?
- What if things don’t go as planned?
- What if I tear?
- OMG what if I poop? (Girl, you probably will – and it’s totally okay.)
You don’t have to just cross your fingers and hope for the best!
Birth It Up unlocks total peace of mind for your big day, so you’re prepared for every possibility!
Erase the unknowns.




Over half of all pregnant mamas are anxious about birth.
But it doesn’t have to be like that for you!
BIRTH IT UP: ONLINE BIRTH CLASSES
Birthing classes for every mama!
Everything in your hospital’s childbirth class – plus so. much. more.
Because every woman deserves to have the knowledge and tools necessary for a positive birth experience – no matter how she delivers.

Natural Birth Class
Eliminate the what-ifs and feel strong and ready for your unmedicated birth.
Start here if birthing without an epidural is your goal!

Epidural Birth Class
Let go of fear and feel fully prepared for (and unafraid of!) your epidural birth.
Start here if you know you want that epidural – or you’re not sure what your birth goals are!

C-Section Birth Class
Release anxiety and gain a sense of control for your C-section birth.
Start here if you have a planned C-section on the horizon OR you want a deep dive on what to expect!

Liesel Teen, BSN-RN
Founder, Mommy Labor Nurse
YOUR CHILDBIRTH EDUCATOR
Liesel Teen, BSN-RN
As a labor and delivery nurse, I’ve spent countless hours with women who felt anxious — even fearful — about giving birth. I want you to know it doesn’t have to be that way for you!
When you know what to expect and have the tools to navigate the experience, you’ll have a better birth — no matter how you deliver.
The three classes in this bundle used to be sold separately – but we realized, that just wasn’t right! Now you can get lifetime access to all three classes for less than the price of one.
Labor and Delivery Nurse of 10 years
Childbirth Educator
Mother of 2
650k+ Instagram Followers

Liesel Teen, BSN-RN
Founder, Mommy Labor Nurse

You’ve got this, mama!
You shouldn’t have to navigate labor and delivery on the fly.
Get the knowledge and encouragement you need to feel more confident and in control starting today.
And know that for every Birth It Up Bundle sold, we’ll donate a bundle to a mama in need!
1. Purchase BIU: All Access
Your purchase is backed by our 30-day money-back guarantee. The only thing you have to lose is uncertainty.
2. Erase the unknowns
Get straightforward information and game-changing tips from a labor and delivery nurse who has seen everything.
3. Have an even better birth
Know what to expect, be ready to pivot your plans if you need to, and feel like the rockstar you are!
FREE RESOURCE
The Mommy Labor Nurse Blog
Check out our searchable blog! You’ll find expert advice, tips, and more for pregnancy, birth, and postpartum.

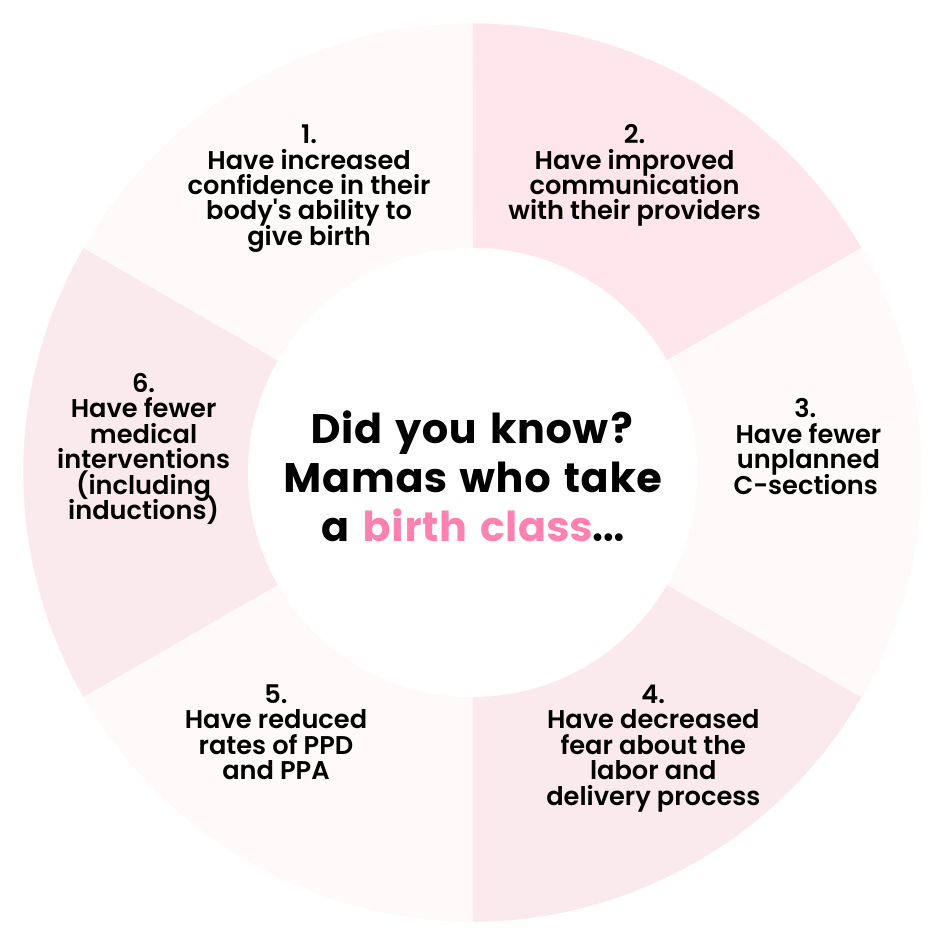
DID YOU KNOW?
Your health insurance might cover the cost of your birth class!
Yaaaas! More and more insurance plans (and nearly all HSAs!) are covering childbirth education.
But because coverage varies so widely – and online info is pretty vague – the best thing you can do is call the number on the back of your insurance card to verify.
The answer just might surprise you!



