In this article, we are taking a look at your C-Section recovery timeline at home. This article picks up after you’ve been discharged!
It provides an overview of what to expect in terms of pain, incision care, and the general postpartum recovery after your C-section birth.
If you are looking for information about the other aspect of your C-Section care, check out these related articles:
Otherwise, let’s dive in!
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
The first weeks of your C-section recovery
Your first week at home is probably going to be tough. I know that’s not what you want to hear, but setting a realistic expectation is important! You are still going to be very actively recovering, feeling quite sore, and dealing with a lot of discomforts. All with a newborn.
But, mama, so many have come before you, and you will be amazed at what you can do! I ALWAYS advocate for lining up lots of support however you can, especially in these first few weeks.
Support in the house is awesome, but even just having meals dropped off, or someone coming in to clean/keep up with laundry is a huge help.
Postpartum bleeding after your C-section
A lot of women are surprised to learn that vaginal bleeding after a C-section is to be expected and is a normal part of your recovery.
Postpartum vaginal bleeding, whether you have delivered by C-section or vagina, is your body’s way of ridding itself of leftover blood, bacteria, mucus, and tissue, something referred to as lochia.
Following a C-section, you may experience lochia for up to 6 weeks. The amount and color of the lochia should diminish over the course of those 6 weeks.
You might notice more bleeding as you increase your activity level in the days or weeks following your C-section. Be mindful of this and make sure you are not overdoing it – your body needs time to heal! Make sure you are following your provider’s recommendations for activity and lifting restrictions.
To manage this bleeding you should use pads only – tampons are not a safe option and can lead to infection!
What to expect at your C-section incision site
So, it is possible that you’ll notice a small amount of drainage from your incision site in the early days following your surgery.
However, heavier bleeding from your incision site is not normal or expected! If bleeding occurs it might indicate a complication, so it’s important to notify your provider right away.
Caring for your incision isn’t too complicated, but definitely something you need to be mindful of to prevent infection and complications.
You can expect to feel some numbness and soreness at your incision site for the first several days or weeks after birth. While the majority of incision pain will go away within several days, the actual site will probably feel tender for several weeks.
It is also normal for your incision scar to be slightly raised or puffy and darker in color than your normal skin tone. As time passes, your scar will become flatter and thinner and return closer to your skin color.
C-section incision care during the first week at home
You will want to make sure you keep the incision site clean and dry so that it can properly heal! The dressing covering your incision site should be removed prior to you being discharged from the hospital.
If your provider has instructed you to leave the dressing on for any reason, make sure to change it once a day, or as instructed, or sooner if it gets dirty or wet.
If you are sent home with a dressing over your incision site, your provider should tell you when you no longer need to keep it covered – try to follow their guidelines as closely as possible.
Let’s take a step-by-step look at how you’ll clean your incision site:
- Make sure your hands are thoroughly cleansed prior to touching or cleaning your incision
- To clean your incision site, wash the area with mild soap and water. It is recommended that you do not scrub the actual site, instead, gently apply soap to the area and let running water rinse the soap off. It is usually easiest to do this in the shower
- To dry your incision simply pat the site with a dry towel. Do not rub the site with the towel as it could irritate the site and cause disruption in the healing process
- If your provider wants you to keep the incision covered, allow the site to fully dry before replacing the dressing
- Air promotes healing in skin injuries, so when possible, expose your scar to air
- Avoid putting any kind of cream, perfume, or bath oil over the site. These are likely to irritate the skin and cause infection
- Do not soak in a bathtub, hot tub, or go swimming until your provider tells you it is okay to do so. This can drastically increase your risk for infection
- If you have steri-strips over your incision, it is also okay to get these wet in the shower. Do not scrub or pick at the steri-strips, they should fall off on their own in about a week
There will be several things to keep an eye on to make sure you are not developing an infection – review these with your provider!
Note: If you notice your incision site opening up or separating at all immediately call your provider. This is a very rare, but very serious, condition known as C-section dehiscence and should promptly be evaluated by your provider.
Pain control in the first week
Unfortunately, C-section pain, especially in the initial 1-2 weeks following surgery, can be fairly intense.
I’m all about setting you up with realistic expectations so that you can plan accordingly and take a proactive approach to your recovery! That starts with learning how to appropriately manage your pain. The good news is that your post-operative pain can be managed in many different ways!
Pain medication
Don’t be afraid to stay on top of your pain medication. You have experienced major surgery and it is completely acceptable to use medication, as directed by your provider, for relief! In other words, don’t be a hero and try to tough it out. I want you to be comfortable, mama.
It is best to stay on a regular regimen so that you don’t let your pain get out of control. It is much more difficult, and very unpleasant, to play catch-up with pain management.
Once you are deep into pain, it will take much longer to feel the effects and relief from medication.
What pain medications are used?
The preferred pain medication recommendations after a C-section are ibuprofen and Tylenol. These two medications can actually be taken together, as prescribed, or can be alternated.
If taken regularly, ibuprofen and Tylenol usually adequately control postpartum pain. Your provider might prescribe a stronger narcotic for you if your pain is not controlled with ibuprofen and Tylenol.
Benefits of keeping up with your pain medication
Adhering to an effective pain medication regimen can actually help you get moving sooner and more frequently! Lack of movement can cause stiffness in muscles and joints which can lead to more pain.
While you might not have the slightest desire to get up and move around, especially during the first several days, it can do wonders for your recovery. Early and frequent movement will also help wake your bowels back up faster, which should mean less constipation and gas pain for you.
I think we can all agree that’s a win!
Let’s review a few more tips to help with the pain:
- Make sure to apply light pressure to your incision if you need to cough, sneeze, or laugh. You can gently press your incision site with a pillow or towel to help lessen the pain.
- Loose-fitting clothes, specifically in the first week or two, will be helpful to avoid anything rubbing against or touching your incision. Loose, soft pants that sit higher on your waist, over-sized shirts, nightgowns, nursing gowns and maternity clothes will provide the most comfort.
- Make sure to follow your provider’s instructions regarding activity and lifting restrictions. This can be exceptionally difficult if you have other little ones at home but it’s so important, especially from a pain management perspective, to not overdo it! Straining your healing abdominal muscles could cause more damage and make your recovery process even longer.
Activity in the first week
During your first week, you will want to take things very easy! We do encourage what’s known as “early ambulation” which means engaging in light activity like sitting, standing, and walking. But this does not mean you should be really active!
It is very normal and recommended to rest a LOT and you should expect to get tired out pretty quickly and easily when you do move about. Make sure you listen to your body and avoid over exhaustion in the first several days and weeks.
Here are a few other points related to your movement in the first few weeks:
- Prior to your 6-week follow-up appointment you should refrain from lifting anything heavier than your baby, roughly 10 lbs
- Avoid exercises that make you strain your abdominal muscles or breathe heavy
- Short walks are encouraged and are a great way to build your strength back up and increase your stamina
- Increase your activity level gradually as to not overdo it or cause over exhaustion
- Most providers will instruct you to not drive for at least 2 weeks following your C-section. Depending on your recovery process, and whether you are still requiring pain medication, this could be longer
C-Section recovery for the next 2-6 weeks
Over the next ~4 weeks, you can expect more of what was described above, with things getting gradually less painful and movement becomes easier. You’ll slowly start to gain back strength and pain will diminish.
Unfortunately, it’s impossible to give you an exact timeline of what this will look like because everyone’s healing process is unique. However, if you continue to keep moving (slowly, while listening to your body), take good care of you incision site to prevent infection or delayed healing, and give yourself plenty of rest – things should be easier every week!
C-Section recovery at 6-8 Weeks
Usually by the 6–8-week postpartum mark most mamas are feeling much better and closer to their “normal” selves. A C-section is major surgery so make sure you allow your body plenty of time to heal.
Don’t stress if you reach the 6- or 8-week mark and still feel like you need some more healing time. Everyone is different and everyone’s body takes different amounts of time to heal, be kind to yourself.
Usually, you will have your follow-up visit with your provider around this time too!
Here’s a look at what you can expect at that visit:
- Getting your blood pressure and weight checked
- A full body assessment, including listening to your lungs & heart, assessing your breasts, and belly
- A pelvic exam (even if you had a C-section), to check your uterus & cervix
- Checking your skin incision. Your provider may want to do this at 2 weeks postpartum as well
- Checking your lab values if you had any medical problems during your pregnancy, such as gestational diabetes or preeclampsia
- Talking about what you’d like to do for birth control, you can get an IUD placed at this time if that’s what you’d like to do!
Postpartum bleeding at 6-8 weeks
By this point, you might still be experiencing a very mild amount of vaginal bleeding (lochia) but it should be very light or scant.
If you are still experiencing any amount of lochia, it should be light pink or white in color, and you should not be passing any clots.
You will still be discouraged from using tampons so make sure to only use a pad or panty liner if you need something.
Incision care at 6-8 weeks
Your incision should require very little, if any, care at this point. Unless you experienced complications, any type of dressing and/or steri-strips should be long gone by now.
It is still a good idea to frequently look at and assess your incision site, it is quite rare, but not impossible to develop an infection at this point.
Pain control at 6-8 weeks
Generally, pain medication is only needed for the first couple of weeks after surgery. With that being said, everyone heals at different speeds and everyone’s pain tolerance is different.
If you are still requiring pain medication at this point, let your provider know at your postpartum visit so he or she can evaluate to make sure there isn’t something else going on.
Activity at 6-8 weeks
At your 6-8 week postpartum appointment, your provider will advise you specifically on increasing activity levels. If your provider thinks everything is healing appropriately, they will give you the okay to start (slowly) resuming certain activities.
Even though your provider might clear you to exercise at this point, it doesn’t mean that your body has completely healed. Make sure you gradually resume activity and slowly work yourself back up to your pre-pregnancy abilities. If you jump back into things too quickly you might set yourself back.
In addition, the restrictions on lifting things heavier than 10lbs should be discussed and removed around this time. Again, make sure you ease back into things! I promise that it is better to wait it out than to risk a major setback (or worse!).
Related Reading: C-Section Recovery Questions You Didn’t Think to Ask
C-Section scar mobilization
Whenever we talk about the C-section recovery timeline, it’s important to chime in with some information about scar mobilization. As you know, during your C-section your doctor cut through many layers of tissue to get to baby. This includes skin, muscle, and fascia – and that requires a lot of healing!
You see, as your body heals all of those layers, scar tissue and adhesions develop. Scar tissue and adhesions (essentially internal scar tissue) isn’t as elastic as normal tissue. It is more fibrous and thick.
Because of this, the different layers of tissue often can no longer slide over each other with ease. In other words, any time you use your core, the difference muscles and tissues cannot contract when needed because the scar tissue and adhesions are inflexible .
This can leave mamas feeling pain in around and their incision site well beyond the expected 6-12 weeks, and it also leads to continued weakening of the core. Some women also experience numbness and tingling here.
This is where scar mobilization comes in
Luckily, there is something you can do to help promote elasticity at your C-section incision site! It’s called C-section scar mobilization. This technique basically massages and moves the tissues in and around your incision site to stretch it out and improve mobility between the different tissue layers.
Typically, you can begin scar mobilization between 6-8 weeks postpartum, but some physical therapists have you start as early as 3 weeks postpartum! I recommend discussing this practice with your provider, and ask for a referral to a PT if you are interested in professional support.
The other great news is that it’s never too late to try it and reap the benefits! Some women don’t learn about scar mobilization until years after their C-sections and they still report benefits from the practice.
How do you do scar mobilization?
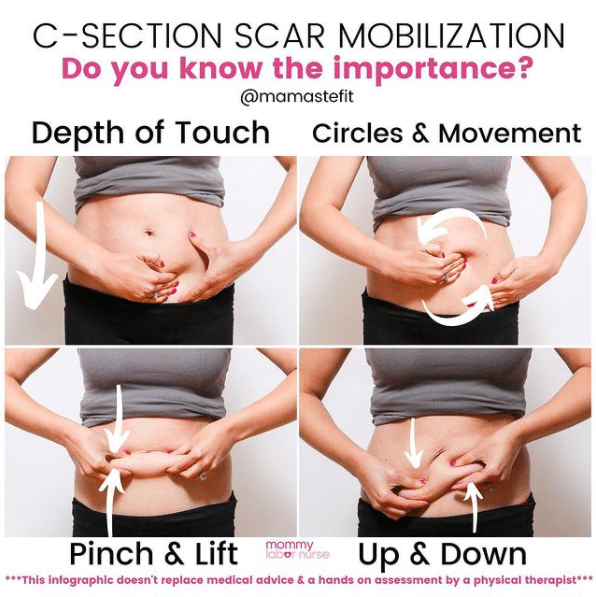
Scar mobilization should not be attempted without medical guidance and a hands-on assessment by a physical therapist. But for educational purposes, I wanted to include some information on what scar mobilization therapy involves:
- First, touch only above and below the scar, then gradually move onto the scar as healing and sensation allow. Explore various textures, such as a cotton ball or fabric, but avoid hot or cold sensations in your exploration
- Explore various depths of pressure; first the superficial layer, or that very top layer of skin. Then deeper into the tissues, and then deepest into the muscle. If you are unsure of appropriate depths, see a PT
- Then explore movement; circles, up and down, side to side, and diagonals at these various depths
- Another technique is the pinch and lift! Grab the scar on each side and lift it from the belly. You may need to grab a wider portion of the abdomen, or you may notice the scar stays lower than the surrounding skin on the lift
- After pinch and lift, you can pull the scar up and down, feeling for any tension or resistance/pulling
Wrapping up
While the recovery from a C-section can feel long and painful, you will get through it! Knowing what to expect, approaching your pain and care proactively, and having a positive mindset will go a long way.
Don’t forget to lean on your support network as needed – it can definitely be a lot on top of the adjustment to life as a new mom.
And if you have any concerns, your provider is always just a phone call away.
For more postpartum support, check out these articles: