Alright, Mama. Today we’re talking all about Group B Strep and pregnancy. Group B Strep is a type of bacteria that’s naturally present in as many as 1 in 4 women!
It’s not harmful to you, but it can cause serious issues for your baby if it infects them during birth. For this reason, Group B Strep screenings are a standard part of prenatal care here in the US.
And with an occurrence rate of up to 25%, I want to make sure you all understand exactly what Group B Strep is all about.
Here we’re going to learn the details about this infection, how GBS disease can impact your baby, and how your provider will screen for GBS. Lastly, we’ll take a look at what it means if you’re GBS positive.
If you do have Group B Strep, your birth will be a little bit different, because antibiotic treatment is highly recommended. Luckily, it’s not as big of a deal as it sounds.
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
What is Group B Strep (GBS)?
Group B Strep is a strain of bacteria that naturally occurs in as many as 1 in 4 women. This bacteria lives in the vagina and rectum, but rarely (if ever) has any negative effects on the women who have it.
In fact, most women are totally unaware they’re “colonized” until their Group B Strep screening comes back positive.

Is it contagious?
According to March of Dimes, Group B Strep is something that’s just kind of naturally present in your body. It isn’t contagious in adults, and it’s not something that you can contract from sex, water, food, or things you touch.
Then why is Group B Strep bad?
The problem with Group B strep is that the bacteria can pass from mama to baby during labor and delivery. This is actually pretty rare, only happening 1-2% of the time.
But, antibiotic treatment is highly recommended to prevent GBS infection to baby because the outcomes for baby can be dire.
How does GBS affect baby at birth?
Okay, so we know that if you have GBS it’s important that it’s not passed to baby, but why is this so important?
When GBS is passed to baby during birth, they are then said to have a GBS infection or GBS disease.
Symptom onset of a GBS infection to baby can occur within the first 7 days of life (early-onset GBS), or later when they are between 7 days and 3 months old (late-onset GBS).
Early Onset GBS in Newborns
With early-onset GBS, symptoms usually present within 12 to 48 hours after birth. This type of infection passes to baby during birth. Antibiotic treatment during labor significantly reduces baby’s risk of contracting a GBS infection during birth, but it’s important to know the warning signs just in case.
Symptoms include fever, drowsiness, and trouble breathing. These symptoms can quickly develop into life-threatening infections including sepsis (blood infection), pneumonia (lung infection), or meningitis (infection of the fluid lining the brain).
Boston Children’s Hospital states that nearly 75% of all GBS infections in babies are considered early onset.
Late Onset GBS in Newborns
Late-onset GBS occurs in babies that are older than 7 days, usually up to 12 weeks old. This type of GBS infection is not passed to baby during birth. Antibiotic use during labor and delivery doesn’t prevent the infection either.
In these cases, it is often unknown how baby became infected with GBS. The U.S. CDC explains that scientists and experts don’t fully understand GBS transmission aside from during birth. But what we do know is that the immature immune systems of very young babies seem to put them at risk.
Symptoms of late onset GBS in newborns include coughing, congestion, fever, drowsiness, and neurological symptoms like seizures. Like early-onset, this infection can cause pneumonia, sepsis, or meningitis.
What if my baby gets a GBS infection?
On the rare chance that your baby does contract early-onset GBS after birth, modern medicine does a really great job of treating these complications.
With treatment, your baby has a 95% survival rate even if they do contract GBS disease. The risk of death is higher among premature babies.
It’s important to be aware of the long term development issues that GBS infection can cause for your baby, even with survival.
In particular, meningitis (an infection of the fluid around the brain) can lead to Cerebral Palsy, hearing problems, learning problems and delays, and seizures.
Does Group B Strep pose a risk to the birthing mama?
It is relatively rare for healthy women to experience any complications from GBS. Remember, this is considered a naturally occurring bacteria after all. However, during pregnancy and birth, it does occasionally cause complications.
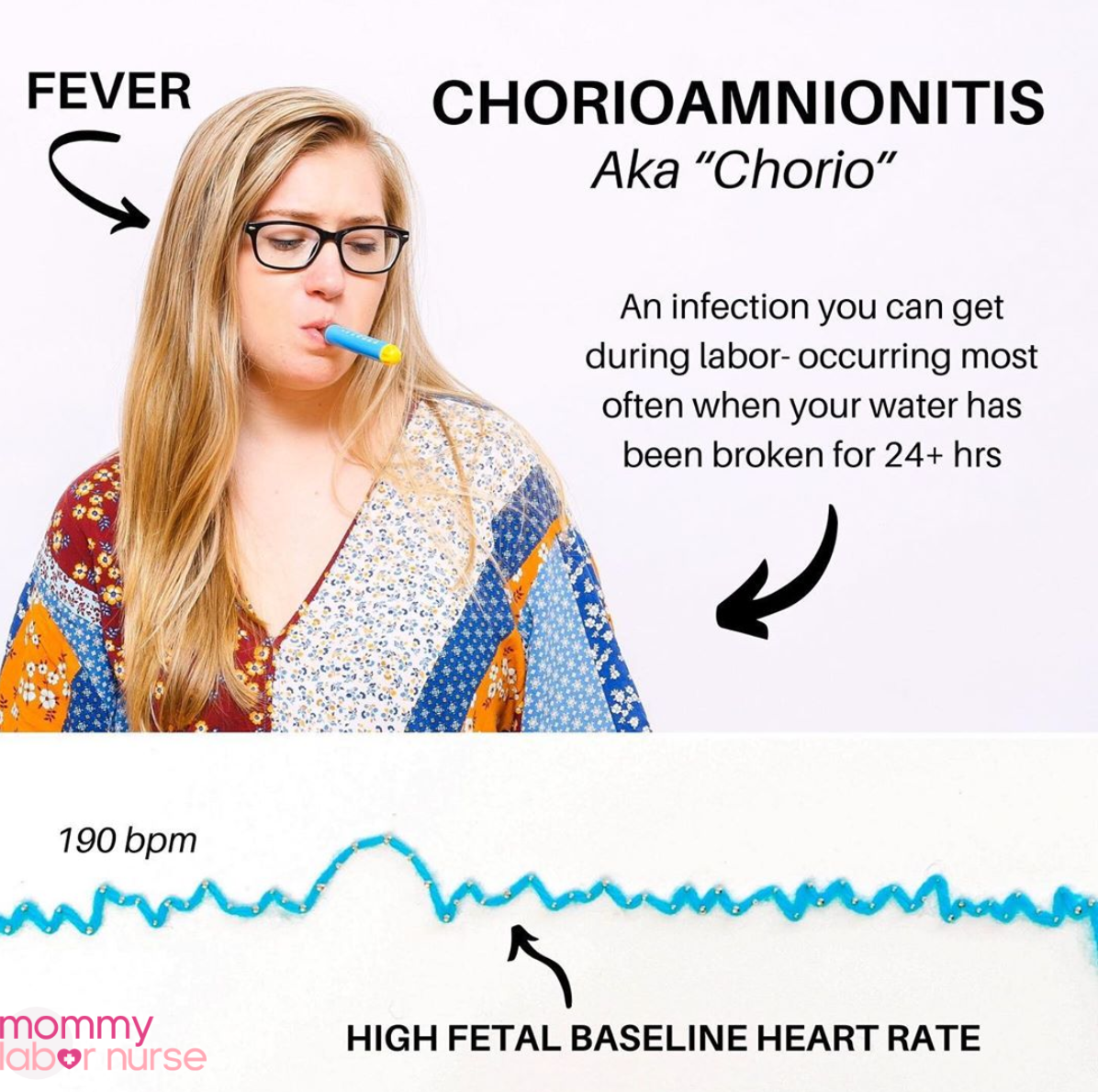
GBS can lead to a uterine infection during or after pregnancy, increased UTIs during pregnancy, and/or a serious infection of the membranes surrounding baby (known as chorioamnionitis).
If you have any signs of infection during pregnancy or during the days and weeks after birth, it’s important to contact your provider immediately! These symptoms include fever, pain in your abdomen, increased heart rate, changes in blood pressure, or anything else feeling off.
When will I be tested for Group B Strep during pregnancy?
Okay, so now that you understand the risks involved with Group B Strep, it makes sense why GBS screening is a routine part of prenatal care, am I right? Antibiotics are highly effective at reducing baby’s risk of infection, so it’s important to know what we’re dealing with.
Luckily, it’s super easy to screen for GBS. The CDC recommends that all pregnant women be screened for GBS between weeks 35 and 37 of pregnancy. Remember, as high as one out of every four women are colonized, so it’s important to check.
Why is the screening at 35 to 37 weeks?
Providers screen for GBS when you are right before (or at) full term because it gives the most accurate picture of whether you are colonized or not. Interestingly, the presence of GBS bacteria can kind of come and go in adult women. Another way of saying this is that GBS colonization can change.
In fact, being GBS positive during one pregnancy, doesn’t necessarily mean you’ll be positive at the next (although this does seem to be the case most of the time). What’s more, you can develop it later in pregnancy, which is why it’s recommended to test so close to your birth.
Group B Strep test: What to expect

The Group B Strep test is seriously no big deal. It’s quick, painless and best of all – highly accurate!
Basically, you or your provider will use a giant swab (picture a giant Q-tip!) to swipe from front to back across your vagina and rectum. It’s then placed in a tube or bag and sent off to the lab to check for the presence of Group B Strep.
It’s that simple!
In some practices your provider or nurse will swab you on the table, but in many others, you’ll be sent into the bathroom with a swab and some simple directions.
What happens if I’m GBS positive?
View this post on Instagram
If you test positive for GBS, you’ll need IV antibiotics during labor to help rid the bacteria from your body and protect baby. The standard safeguard is that you’ll need IV antibiotics at least 4 hours before you deliver. This gives the IV medication enough time to get to baby and provide protection, if baby is exposed to the GBS bacteria during labor and delivery.
According to the CDC, if you receive these antibiotics during labor within 4 hours of delivery, baby’s chances of contracting GBS infection is about 1 in 4000 (as opposed to 1 in 200 if antibiotics aren’t administered!).
A lot of mamas wonder why they can’t just take antibiotics leading up to birth…why does it have to be an IV?
Unfortunately, GBS grows back quickly. The only way to knock it out for the entire labor and delivery is with antibiotics administered via IV.
Group B strep positive when to go to hospital
So, if you’re GBS positive, you know that we ideally want to get you a dose of antibiotics within 4 hours of delivery. As you probably know, it’s impossible to predict how long any woman’s labor is actually going to be!
Usually the guidance is that if your water breaks and you are GBS positive, you need to come right in! This is because after your water breaks, labor can ramp up really quickly (but it’s not always the case).
Otherwise, if this is your first birth, the guidance isn’t too different. Most providers say it’s safe to wait to come in until you are in strong, active labor.
If this is a subsequent birth, you may want to err on the side of caution and come a bit sooner than the standard 4-1-1 (contractions 4 minutes apart, lasting for a full minute, for at least one hour) just in case things progress rapidly.
As with most things like this, you’ll need to ask YOUR provider the right plan for you.
What happens if I don’t make it to the hospital in time to administer antibiotics?
If for some reason you do not make it to the hospital to get your IV antibiotics in a timely manner, it’s OKAY! Yes, your baby is technically at an elevated risk for infection.
Luckily, modern medicine is highly effective, and you will be in the best hands for observation should symptoms arise!
In most hospitals, what will happen is they will want to watch baby in the hospital for any symptoms for at least 48 hours. It’s possible that this can lead to a slightly longer-than-average hospital stay.
They also MAY want to draw labs to see if baby’s blood counts indicate any signs of infection.
What’s birth like if you have Group B Strep?
There is a common misconception that if you’re GBS positive you have to be hooked up to an IV for your entire birth. Well, I’m here to tell you that’s 100% not true!
IV infusions are only 30 mins, so you can get the antibiotics, and then if you wish to be disconnected from the tubing, that’s totally fine! However, if any other IV medications are needed (like IV fluid, Pitocin, or Magnesium Sulfate) you may have to remain connected to the IV pump.
This means you can still totally utilize any and all labor positions and pain coping strategies you want to have your best birth! This will be especially important if you are planning for an epidural-free birth.
Related Reading: 25 Tips for A Natural Birth
Tips for you and baby if you’re GBS positive
Having GBS at birth is certainly not the end of the world. In fact, we’re very fortunate that it’s so easy to identify and that effective treatments exist. Anything that can reduce the risk of complications in our sweet newborns is a seriously amazing thing!
However, I totally get that some mamas are bummed out about the idea of antibiotic use during birth – even if it doesn’t really impede the actual event too much.
Are there negative impacts of antibiotic use during birth?
You see, some research does indicate that antibiotic use during labor can delay the immediate production of healthy gut bacteria in babies. But the same research shows that by 12 weeks, their gut bacteria is just as developed as babies that weren’t subject to antibiotic use.
There is also some very new (and interesting) research occurring about the early development of a healthy microbiome and its effect on metabolic and immunologic processes later in life (source).
This may indicate a link between microbiome development delays and an increased risk for diseases such as obesity, allergies, inflammatory bowel disease, and even some cancers. I bring this up with a huge disclaimer that this research is very new and contains a LOT of unknowns.
And above all else – the use of antibiotics for the prevention of GBS infection FAR outweigh the negative impacts of antibiotics, so I am in no way suggesting you skip them if you are GBS positive!
What can I do to mitigate the effects of antibiotic use during birth?
One of the best things you can do is practice LOTS of skin-to-skin care and breastfeed, if possible.
There’s a lot of fascinating and positive research that shows how skin-to-skin care and breastfeeding can support the development of a healthy microbiome in C-section babies. And the same school of thought supports that it can help babies born under antibiotic use, too!
What’s more, YOU can probably benefit from taking a probiotic after birth, too. Like baby, your gut bacteria may be kinda wiped.
Some women also may be at an increased risk to develop thrush after heavy antibiotic use or have digestive issues. A probiotic can help with this!
Group B Strep unpacked
Well, Mama, there you have it! Whether your GBS test is at your next appointment, or you’ve been deemed Group B Strep positive you’ve now got the whole lowdown on why this screening is so important.
As you now know, antibiotics are a wonderful line of defense against infection. A positive screening means that your provider can make sure you and baby receive the best possible care to keep you both safe during delivery!
Were you GBS positive? How did it affect your birth experience? I’d love to hear about it in the comments below!
Happy Birth!