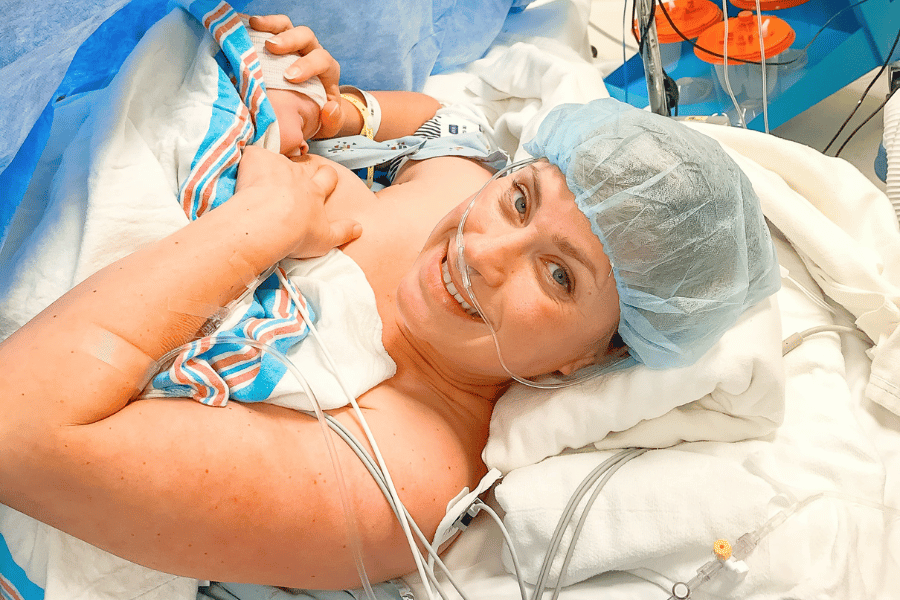
Hey mama! As you prepare for your little one’s arrival, you’re probably making lots of decisions – from choosing a car seat to picking out the perfect crib. But have you thought about what happens to your baby’s umbilical cord and placenta after birth?
These often-discarded treasures actually hold incredible potential! As always, this article is meant to inform you to make the right decision for your birth and your family. I encourage you to take this information, do your own research, and discuss this decision with your OB provider before giving birth.
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
Cord blood banking
The blood found in your baby’s umbilical cord is full of stem cells that could possibly be used to cure your baby or family member of a disease one day. The vast majority of babies, however, won’t end up ever needing their cord blood, and current technology greatly limits how useful it really is.
Choosing to bank your baby’s cord blood is a very personal decision that is typically made after lots of research and discussion. There are many factors to consider, including cost, when making this decision.
What is cord blood banking?
Cord blood banking involves collecting and storing the blood from your baby’s umbilical cord after birth. This blood is extra special because it contains stem cells which are basically little tiny cell superheroes!
Role of stem cells
Stem cells, which are found in almost all tissues of the body, are unique and special for a couple of reasons. “They are able to make more cells like themselves. And they can become other cells that do different things in a process known as differentiation.” (source)
The stem cells present in cord blood are especially unique! They are rarely rejected during transplants, they present more possibilities for matches than bone marrow, there are 10 times more stem cells present than in bone marrow, and they can be frozen for an indefinite amount of time before being used.
Cord blood storing options
When it comes to storing cord blood there are two main options.
Public cord blood banks
Public cord blood banks are free to donate to. Upon receiving the cord blood, the public bank will run tests on the blood. They will then catalog it into a registry that doctors can access for use in patients in need.
Public cord blood banks contribute to furthering research on the potential benefits of cord blood and their use can provide life-saving cells to people in need across the country.
To donate to a public cord blood bank:
- Your blood will need to be prescreened to ensure it is free of genetic disorders and infectious disease
- You need to give birth at a certified cord blood collection site (which many hospitals are!)
- The blood to be donated also must be at least 40 mL, which means delayed cord clamping is likely not an option because delayed clamping won’t allow enough blood to stay in the cord (though you should discuss this with your provider!)
Private cord blood banks
The other storage option is in a private family bank. In this scenario, your baby’s cord blood will be stored for baby’s use or for direct family donation. Private storage banks charge a fee for collection and a monthly or yearly storage fee after. Private storage banks market their services as “biological insurance for your child and family”.
But I want to be transparent in telling you that this claim is rejected by the American Family of Pediatrics and the organization strongly cautions parents against their use.
Benefits to banking cord blood
Benefits of public cord blood banks
- Your baby’s cord blood will be cataloged into a registry available to all doctors looking for stem cells to save their patients’ lives
- The stem cells in your baby’s cord blood might be used to advance medical research or in life saving clinical trials
- Donation is completely free
- Donating cord blood to a public bank is contributing to the advancement of this field of research and to the “good of science” and “greater good” if you will
- For those interested in cord blood banking, this is the method most often recommended by the AAP and ACOG
Benefits of private cord blood banks
- Privately stored cord blood is stored just for your baby and your family’s use
- The cord blood may be used to treat a sick family member or in the event of a family member needing a stem cell transplant
- If you have a sick family member that needs, or may one day need a stem cell transplant, you may be making a lifesaving choice by storing cord blood privately
- There is an ever-changing and evolving understanding of how stem cells and cord blood can be used, in the future it may benefit your baby in a way not currently known
- Private cord blood storage is only recommended by ACOG and the AAP if you have a family member with a known disease that will benefit. Otherwise, it is not recommended. The idea of “biological insurance” is rejected and seen as a marketing tactic
Drawbacks to cord blood banking
- You can’t do delayed cord clamping: You often cannot do delayed cord clamping (DCC) if you are donating to a public bank because not enough blood can be collected. If you’re donating to a private bank you can do DCC but the amount of blood collected in that case will be limited in its potential benefits especially considering the storage cost
- Private cord blood storage is costly: This varies from facility to facility, but fees average around $2000 for initial processing and have an annual fee between $100-$300
- Private cord blood storage is not recommended by the AAP unless medically necessary: For a variety of reasons, the American Academy of Pediatrics does not routinely recommend private cord blood storage (read more here). The same claims are supported by ACOG (read here)
- Cord blood can currently be stored for 20 years: For this reason, it really makes sense to contribute to a public bank. Blood stored in a private bank will only give your child that “biological insurance” for 20 years
- Most privately banked cord blood is never used: According to the Cord Blood Association, the chances of your baby ever needing their own cord blood is very low and WebMD cites a study that says the likelihood is between 1 in 400 and 1 in 200,000. One reason for this is that in the event of blood cancer, like leukemia, a baby’s own cord blood cells cannot be used to fight the disease. The likelihood of a family member using your child’s stored cord blood is also very low. This is because the amount of stem cells in a single cord blood collection is not enough to support a transplant in most adult patients
Placenta donation & encapsulation
Okay, so moving along from the cord…let’s talk about what you’ll do with your placenta! Standard protocol after you deliver your placenta is disposal by the hospital.
However, there are actually some options here:
- You can choose to take your placenta and have it professionally encapsulated for consumption
- Donate your placenta for research
- Bring your placenta home for raw consumption (not recommended)
- Take your placenta home to plant it, have it made into jewelry, or create art with it
Placenta encapsulation
For centuries and across many different cultures, women have been consuming their placenta to benefit themselves postpartum. However, in today’s day and age, it is very controversial because it doesn’t come without risk.
It’s important to note that 70-80% of moms who choose to consume their placentas choose encapsulation. However, it can also be eaten raw (not recommended!), cooked, dehydrated, or roasted.
Placenta encapsulation involves steaming the placenta, drying it out, and then grinding it up into a powder and placing it in capsules. Typically, this is done by a professional service.
It’s so important to make sure the placenta is handled safely. It should be packed in ice right after delivery, be stored correctly, and cooked thoroughly before consuming. There are no laws governing the practice of placenta encapsulation. It’s important to do adequate research and choose a company that will handle the placenta safely.
Potential benefits:
- Increase in milk production
- Restoration of blood iron levels
- Increased release of oxytocin, which can help the uterus return to normal size and encourages bonding with baby
- A decrease in postpartum depression
- Increase in CRH (corticotropin-releasing hormone), a stress-reducing hormone
Potential risks:
- Improperly encapsulated placentas can harbor bacteria that can make you sick – and baby if you are breastfeeding
- Exposure to environmental toxins, like heavy metals, that accumulate in the placenta during pregnancy (this is because the placenta acts as a filter for baby while they’re in the uterus)
- Lower milk supply – the placenta contains progesterone, which inhibits the production of prolactin
- Increases risk of developing blood clots – the placenta contains estrogen, which increases the levels of clotting factors in the blood
- Can cause jitteriness/dizziness
I want to note that the pros and cons listed out here are largely based on anecdotal evidence! But there have been few studies done on the risks/benefits of placenta encapsulation.
Donating your placenta
In my experience, placenta donation is talked about a bit less than some of the other topics in this article. It is the act of donating your placenta for research or medical use.
Placenta donation is something that you’ll be asked about once admitted to the hospital. You will need to:
- Give consent
- Complete a medical history form
- Have your blood screened for any diseases that could be passed to a receiving patient through your birth tissue
Why donate your placenta?
As I mentioned above, your placenta is typically discarded after birth (unless you opt to take it home with you). Placenta donation doesn’t impact your birth in any way.
It isn’t taken until after baby has been delivered safely and doesn’t affect your ability to opt into DCC or cord blood banking.
Keep reading to learn more about specific placenta donation benefits!
Placenta donation benefits
In short, donating your placenta truly doesn’t affect you or baby at all! The tissue from your placenta and cord, referred to as birth tissue, is currently used to:
- Heal traumatic wounds
- Aid in skin grafting for severe burn victims
- Assist in the treatment of diabetic ulcers
Doctors and researchers are finding more and more benefits and uses for birth tissue too. This includes helping patients with eye injuries and diseases, spinal and dental procedures, and sports injuries as well.
You can learn more about the process, benefits, and how to sign up at Birth Tissue Recovery, and/or ask your provider for information at your next prenatal visit.
Remember, Mama:
Whether you choose to donate, bank, or discard your placenta and cord blood is personal. The decision is entirely up to you and your family. There is no right or wrong answer here so try to not let other’s opinions and decisions sway your own.
I do encourage you to start having these conversations and doing your own research early on in and prior to pregnancy. Decisions about cord blood banking and placenta donation should be made well before your little one’s arrival so make sure you are giving yourself plenty of time!