When it comes to talking about birth, epidurals are often a part of the conversation in one way or another. And I’d guess that most of you already know that epidural placement eliminates labor pain.
But beyond that? Well, a lot of people don’t actually know that much!
I often get questions about how epidurals are placed, how big an epidural needle is, if getting an epidural hurts, and lots more! So today I thought we’d unpack these epidural placement FAQs that show up in my DMs.
Because whether getting an epidural is part of your birth plan or not, I highly recommend all pregnant women learn as much as they can about epidurals. You see, sometimes plans change once labor begins and the more you know about every possible option – the better.
As a labor and delivery nurse, I’ve seen hundreds of epidurals, so if you’re curious about how it all goes down, read on to learn more!
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
What is an epidural?
Quite simply, an epidural is an injection that is placed in the epidural space of your back to eliminate pain. The epidural space is one of the areas that surrounds your spinal cord. And the epidural placement is always done by a provider on the anesthesia team rather than your delivery provider.
Epidurals are often referred to as the “gold standard” when it comes to pain management during labor and birth because of their seemingly magic ability to eliminate most (if not all) of the pain sensation that comes with birth.
Epidural catheter
Many people think an epidural is a one-time shot in the back and that nothing stays – but that’s actually not the case. Having an epidural during labor requires placement of a long, wire-looking catheter in your back.
This epidural catheter is about 90 centimeters long, but only 10-12 cm will actually stay in your back. The other end of the catheter will be connected to a pump that continuously distributes medication. In other words – this is how the pain relieving magic *actually* happens.
Wait, so how exactly does an epidural work?
An epidural works by blocking pain signals that travel from your spinal cord to your brain. The goal of an epidural is to provide temporary numbness from contractions by blocking the signal of the pain!
Now, since the pain signals are being blocked, I want to warn you that you’ll still probably feel pressure.
You see, as baby descends lower into your pelvis, a lot of pressure occurs in your pubic bone and rectum. Some women with epidurals don’t feel this sensation, while others feel extreme pressure and even some pain.
Epidurals are actually not intended to take away pressure. And actually, pressure is a good thing because it can help guide pushing! So if you feel pressure, don’t panic that your epidural has stopped working. Instead, when it’s time to push you can focus on that pressure to push more effectively.
When is the best time to get an epidural?
The million dollar question! Which unfortunately, I cannot provide a cut and dry answer for. Because contrary to popular belief, there is no magic number of centimeters dilated, or number of hours into labor you must be in order for you to get an epidural. The best time is truly unique to each mama and birth.
However, I’m not going to leave you totally hanging! There are some clues to help you decide when the best time is for you. In my experience, these 3 things should be happening before you get an epidural:
- You should be having painful contractions
- Your cervix should be dilating
- You should not be pushing your baby out
Basically, if you are having painful contractions that are dilating your cervix, feel free to ask for an epidural whenever you feel ready for it – could be at 3 cm or 9 cm!
Keep in mind that it can take some time for anesthesia to place the epidural once you request one. Depending on the size of the hospital where you are delivering, anesthesia may or may not be on site 24/7.
When is it too late to get an epidural?
As long as you can sit still enough to safely have the epidural placed, you should be able to get one! However, it takes about 30-45 minutes to get your IV fluid going, supplies together, and an anesthesia team member to the bedside, so make sure you account for this when asking for your epidural.
It can also take an additional 20-30 minutes to feel the full effects from the epidural once it’s placed. So even if you can sit still long enough to have it placed, there is a chance it might not have time to kick in if your labor is progressing quickly.
Epidural placement process
Alright, now let’s talk about the actual epidural placement. This is the part that gives a LOT of women anxiety. And listen, I get it. Needles can be scary, but I promise that this isn’t as bad as it seems in your head.
Let’s go through it step-by-step to erase the unknown of it all and get you feeling more confident.
Step 1: Epidural preparation
Before you can have your epidural placed, there are a few things that need to get done. Though if you request an epidural after you’ve been admitted, most of this will already be done.
But if you have just arrived at the hospital and immediately request an epidural, here’s what you can expect:
- IV access
- One of the most common side effects from an epidural is hypotension, or low blood pressure
- One way we counteract this blood pressure drop is by giving you extra IV fluid
- If your blood pressure still drops despite the additional fluid, we can give you other medications through your IV that will quickly bring it back up
- All of this to say that having an IV prior to an epidural placement is a definite must
- Bloodwork
- While placing your IV, we will also collect some blood to check your platelet count
- Low platelets are a contraindication to getting an epidural so we must have this information before it can be placed
- Depending on the facility, it should take roughly 15-30 minutes for your results to come back once the lab receives your blood sample
- IV fluid
- IV fluid is given before your epidural placement to try and avoid a significant drop in your blood pressure
- Some anesthesia team members want the whole bag of IV fluid to be infused before they will place the epidural, while others are ok with placing it as long as the fluids are actively running
- It can take anywhere from 20-60 minutes to receive a whole bag of fluids
- Gather supplies
- Your nurse will be in charge of gathering the supplies that will be needed to place your epidural
- Once everything is set up, anesthesia will be called to your room to do the actual placement!
Step 2: Giving consent
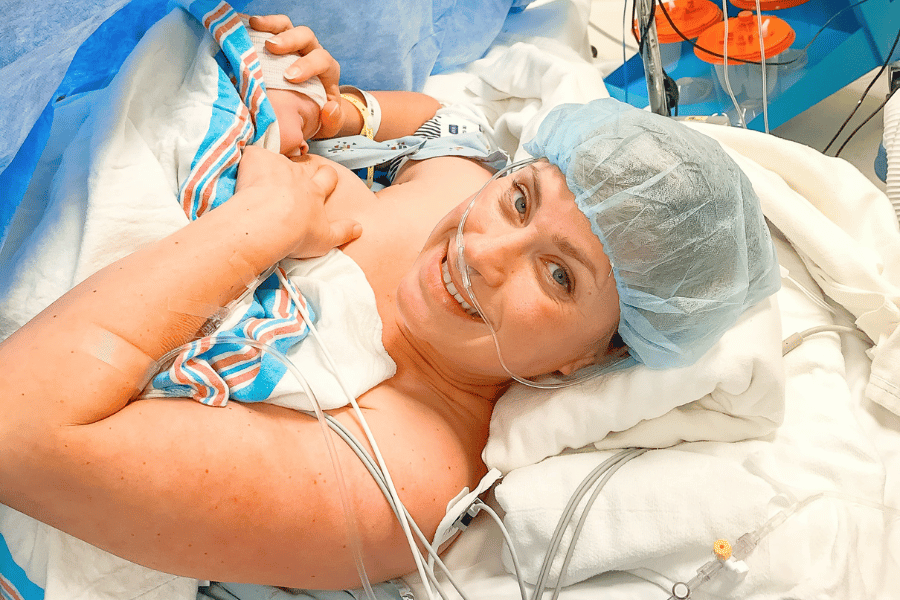
Relief is on the way! When anesthesia arrives we will get you into position. Depending on anesthesia’s preference, you will either be sitting on the side of the bed with your legs dangling or lying on your side.
Once they arrive, the anesthesia team member will briefly explain the procedure, including risks and benefits, and give you a chance to ask questions. Remember, if you are in painful, active labor, this conversation will very likely be quick and to the point. For this reason, it’s a good idea to discuss any epidural questions and concerns you have before you’re even in labor (like when you make your birth plan!).
When this is done, they will have you sign a consent form, giving them permission to place the epidural!
Related Reading: How to Make a Birth Plan: An L&D Nurse’s Guide
Step 3: Sitting for your epidural
As soon as you give consent, we will be begin sterilizing your back. A blood pressure cuff and pulse oximetry probe will be placed on your arm and finger to monitor your vital signs.
Now, your positioning during the epidural placement is SUPER important so here’s a quick overview of how to sit for your epidural:
- Sit very slouched
- Touch your chin to your chest and slump your head down in front
- Relax your shoulders
- Relax your arms in your lap
- Think about curving your back like a shrimp or mad cat
Step 4: Placing the epidural
Once you are in the correct position, your back will be cleaned with an antiseptic solution and a sticky drape will be placed on your back.
Next, you will feel the anesthesia team member pushing on your back to determine the best spot for placement.
When they find it, they will insert a small needle to numb your back. This normally feels like a bee sting and is often the worst part.
As soon as your back is numb, a larger needle will be inserted into your back and slowly positioned into the epidural space. The depth the needle needs to go in to hit that spot varies based on the individual and their body type, but it’s usually in the range of 4-8 cm (source).
Once the needle is in the right spot, the anesthesia team member will thread a catheter into your back and take the needle out. Remember, the wire-looking catheter is super long (about 90 cm) but only about 10-12 cm of it stays in your back.
The remaining amount is used for slack to hook up the pump that will continuously give you medication throughout your labor.
Step 5: Testing the epidural
Next, anesthesia will give you a test dose of medicine to make sure the catheter is in the right place. If it’s in the wrong space, it might need to be removed and replaced (luckily, this doesn’t happen too often!).
This whole process of steps 3-5 normally takes about 10-15 minutes (sometimes longer if there are difficulties getting the needle into the epidural space).
The very last thing is to tape the epidural catheter to your back and give you a bigger dose of numbing medication. Some women feel relief within 5 minutes but for most it takes 15-20 minutes and is more of a gradual progression.
Related Reading: 12 Important Epidural Side Effects and Facts You May Not Know!
How big is the epidural needle? What’s the epidural needle size and length?
This is another very common question. And the truth is that the epidural needle size and length varies depending on the size of the patient. The most common epidural needle size is a 17 or 18-gauge needle. Gauge refers to the diameter of the needle. The higher the gauge, the smaller the diameter.
The typical epidural needle length is about 3.5 inches for a normal-weight adult and up to 6 inches for an obese adult.
Does getting an epidural hurt?
I touched on this previously, but most people say that the worst part of an epidural placement is the numbing medicine. I haven’t personally gone through this experience, but a lot of people say that the numbing medicine feels like a bee sting.
You can expect to feel some pressure in your lower back as the epidural needle is inserted. You also might feel a sensation shoot down one or both of your legs (it feels like you hit your funny bone!) as the catheter is being threaded.
If you are experiencing pain with the placement, let your anesthesia provider know promptly so they can address it.
How long does an epidural last?
Once we determine your epidural is in the right place, the epidural will be taped to your back. Then the catheter will be connected to a pump that will continuously infuse pain medication until you deliver. This means that you should have adequate pain relief from the epidural throughout your entire labor.
As I previously mentioned, it’s not uncommon, even with a perfectly functioning epidural in place, to feel a pressure sensation (sometimes very intense) as baby moves down lower into your pelvis and gets closer to coming out.
The epidural is meant to take away sharp contraction pain but is not meant to take the pressure sensation away. Pressure helps guide your body when and how to push when the time comes.
Wrapping up
Whether you plan on getting an epidural from the moment you find out you’re pregnant, or hours deep into labor, it’s important to be informed about the procedure.
In fact, even mamas who plan to go natural should get education about epidurals in case they change their plan once they’re in labor. This is exactly why I teach about them in my natural birth course!
I recommend exploring ALL the pain medication options for labor, even if your intention is to have an unmedicated birth!
Check out the blog articles below to learn more:
- A List of Pain Meds During Labor Other Than Epidurals
- Everything You Need to Know about Walking Epidurals
Or these posts over on Instagram: