Hey Mamas! This week I’ve put together a post outlining the basics of how to prepare for labor induction through my eyes as an L&D nurse.
It’s for the mamas who KNOW they’re getting induced (for one reason or another) but also for the mamas who AREN’T expecting a labor induction AT ALL…because many times inductions are unplanned!
We’re gonna talk all about what labor induction is, different induction methods (like Cervidil and Foley bulbs), how to prepare for labor inductions, Pitocin side effects, and a whole lot more.
Consider this your complete guide to labor inductions! Are you ready? Let’s go!
- What is a labor induction?
- How to prepare for labor induction: learn about different methods
- How to prepare for labor induction
- Starting the Pitocin
- Dos and Don’ts Before Being Induced
- Things to do before your induction:
- Things not to do before your induction:
- Those are your dos and don’ts before being induced!
- How else can I prepare for labor induction?
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
What is a labor induction?
An INDUCTION OF LABOR is exactly what it sounds like…you aren’t in labor, so we put you into labor (or we ATTEMPT to put you into labor).
Reasons for labor induction
- Overdue (most practices consider this to be past 41 weeks, but many nowadays wait even longer, up until 41 & 6 days)
- Preeclampsia
- Gestational diabetes
- Baby has IUGR (intrauterine growth restriction)
- You’ve broken your water early in your pregnancy
- History of stillbirth
- Cholestasis
- Any other medical condition that puts you or baby at risk to continue your pregnancy safely
Augmentation of labor
NOW, inductions differ from augmentation of labor. Augmentation of labor is done when you’re already in labor.
Here’s an example of labor augmentation:
- Let’s say you’re contracting, you get an epidural, and your contractions space out after you get comfortable with your epidural
- It’s been a few hours, and your cervix hasn’t changed
- Your provider may suggest starting some PITOCIN, or BREAKING YOUR WATER. This isn’t a labor induction, this is an augmentation
Augmentations are similar to inductions, in that the methods are the same, but we’re more just helping your labor instead of starting it.
Related Reading: Epidural Facts You May Not Know
How to prepare for labor induction: learn about different methods
Labor inductions can be done in MANY different ways. In fact, I’ve already referenced two above! PITOCIN and BREAKING YOUR WATER.
I’ll go over all the methods that we use at my hospital (and a few others that I’m aware of).
1. Pitocin
Pitocin is a medication that’s given through your IV to get your labor started. This is by far the most common labor induction method!
It’s the man-made form of the same hormone your body naturally produces when you’re in labor…oxytocin. By giving you oxytocin synthetically, we are attempting to tell your body that you’re in labor!
Every hospital is different (and every nurse is different), but generally Pitocin is started at a very low dose (usually only 2ml/hr, which is less than half a teaspoon) and titrated up to a certain threshold. This threshold is different for every woman.
At my hospital, we may max our patients out at 40ml/hr of Pitocin, and we are only allowed to increase the dosage by 2 ml every 15 minutes. I’ve heard of many hospitals that only allow their nurses to max out their patients at 20ml/hr, however.

What a Pitocin induction may look like
If you started your labor induction at 8 am, and your nurse was ON IT, increasing your Pitocin EVERY fifteen minutes, you’d be at 40ml/hr around 12:45 pm
Now, not every woman needs 40 ml of Pitocin to get into labor.
In fact, MOST women need much less to have an adequate labor pattern. It all depends on the woman, her gestation, her uterus, how irritable her uterus is, HOW BABY IS REACTING….and so on.
How we administer Pitocin at my hospital
My hospital policy allows us to increase Pitocin every 15 minutes until contractions are in an ADEQUATE labor pattern. This usually means, they are 2-3 minutes apart, painful, and CHANGING YOUR CERVIX.
That’s a big one. You can be having crazy, long, painful contractions coming every 2-3 minutes, but if your cervix isn’t changing…I’m going to keep increasing your Pitocin.
Things I’m looking out for during a Pitocin labor induction
- First off, I don’t want your contractions to be TOO close together. Your uterus needs to adequately relax in between your contractions before you have another. This cannot only stress out baby but it also increases your risk for something really scary called a uterine rupture. Yuck, you don’t want that. So just know, if I see your contractions are a little bit TOO close for TOO long…I’m going to back down your Pitocin
- Second, Pitocin can be stressful to baby (any labor, in general, can be stressful for baby), and if I ever see baby getting stressed out (as evidenced by his/her heart rate), I’m going to back down your Pitocin…or shut it off completely. Ain’t NOBODY got time for a stressed-out baby!
2. Breaking your water
Alright! This is the second most common way to attempt labor induction. Also, I must add…during your labor induction, you may have SEVERAL different methods used. Totally common and okay!
Breaking your water is a form of induction, and I’ve heard of many hospitals using this method FIRST, as a means to get labor started.
We don’t typically do that. Usually, breaking your water is something that we use in conjunction with Pitocin. It’s usually done later, after you’ve been contracting for some time and baby’s head is low and well-applied to your cervix.
This is when it WORKS THE BEST.
How does breaking your water help move labor along?
- It helps to bring baby down into your pelvis, creating more pressure on your cervix. This increased pressure helps your cervix to change!
- Releases PROSTAGLANDINS around your cervix (magical labor-inducing hormones), this stimulates cervical change!
Related Podcast: Will I Poop During Labor?
Related Reading: What to Expect the Day of Labor
3. Foley bulb
View this post on Instagram
A Foley bulb is a little catheter that’s manually inserted inside your cervix to DILATE it manually. It also provokes your body to release some prostaglandins (labor hormones!) around your cervix.
They work really great if they are used properly and in the right circumstances.
Now, USUALLY, Foley bulbs aren’t meant to do the job on their own. I have seen some women get a Foley bulb placed, and they start contracting and have a baby WITHOUT Pitocin.
But, 90% of the time you’ll get a Foley bulb placed, in addition to getting Pitocin started (typically a little later in the game).
What is a foley bulb?
- A Foley bulb is a long, flexible catheter about the thickness of a McDonald’s straw (you know how they are a little thicker than normal straws)
- It’s nice and bendy, and it’s usually made of latex or a similar material
- It’s got an opening on one end, and the other end is a BALLOON-TYPE mechanism that can be filled with fluid (this is the part that goes in your cervix)
How is a foley bulb placed?
First off, NO NEEDLES go inside you. A needle is used to draw up the fluid that is used INSIDE the end of the Foley bulb, and sometimes women get a little nervous at seeing the needle in action. No worries, it’s not going anywhere near you!
- Your provider will have you lay on your back with feet in stirrups (just like during a pap smear or vaginal exam)
- They’ll use their hands or a speculum to place the Foley bulb in your vagina
- Then it is moved through your cervix. This can be a bit uncomfortable (you might feel lots of cramping, and may have some contractions after the procedure)
- Once your provider has the balloon part of the Foley bulb through your cervix, your nurse will fill the bulb with water until your provider says to stop
- Once it’s filled up, it stays in your cervix for anywhere from 30 minutes to 12 hours. I know, that’s a REALLY long range, but it all depends on HOW dilated you were to begin with and if you have any contractions while the Foley bulb is in
- Typically, if you are having your first baby and your cervix is 1 cm dilated or less, your Foley bulb will stay in overnight…PREPPING your cervix for labor the next day
But remember, sometimes we use Foley bulbs and Pitocin at the same time – it all depends on your circumstance!
We do Foley bulbs A LOT at my hospital, but I’ve also heard of certain hospitals not using them AT ALL. It just depends on your provider and his/her preference. Many providers use medications that are inserted in your cervix (which I’ll get to in a moment), instead of placing a Foley bulb.
4. Cervidil and other medications
There are a couple different medications that can be used at the beginning of labor induction. Most of them are inserted vaginally and work to PREP your cervix.
These medications all help your cervix relax so that it can open more easily. This is in contrast with something like Pitocin which has the goal of starting rip-roaring labor contractions.
The most common intravaginal medications are:
- Cervidil: this is a prostaglandin that’s inserted vaginally. It helps relax the cervix prior to the induction of labor
- Cytotec: another prostaglandin that’s inserted vaginally to help kickstart labor
- Laminaria: this is actually derived from seaweed (who knew!?) and contains thyroid hormones. It is used in labor to help ripen and open the cervix
Related Reading: How to Induce Labor Naturally
How to prepare for labor induction
ALRIGHT, so now that we’ve gone over WHAT a labor induction is, WHY you’d get induced, and WHICH method your provider might use, let’s go over HOW it all goes from my perspective!
You’ve got your labor induction date scheduled, and you get a phone call from the hospital! WE ARE READY TO MEET YOUR BABY!
If you’re a first-time mom, you’ll probably come to the hospital at night to get your cervix “prepped” for labor with a Foley bulb or intravaginal medication.
If you’ve had a baby before, you’ll probably come in the morning.
Related Reading: Hospital Bag Checklist
1. Arriving at the hospital for your labor induction
Once you arrive at the hospital, you’ll go through registration and be brought up to labor and delivery. Your nurse will meet you in your room, and ask you a few preliminary questions…
- Have you been having any contractions?
- Have you been leaking any fluid?
- Has baby been moving around well?
- Have you experienced any bleeding?
Once you answer these questions and we determine there’s no immediate health threat to you or your baby, your nurse will ask you to undress completely, provide a urine specimen, and change into a gown.
Related Reading: Trying To Go Natural? A Few Tips From An L&D Nurse
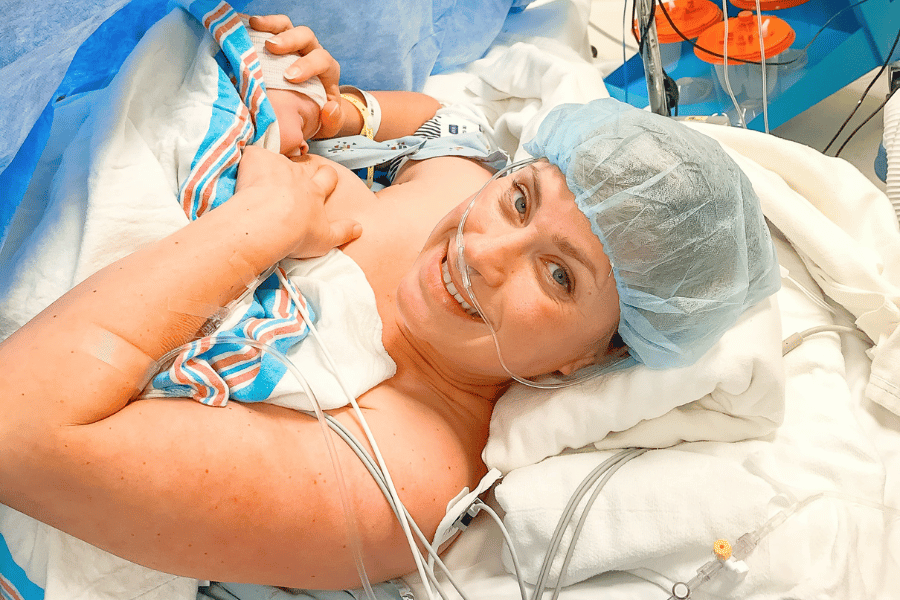
3. Setting up and monitoring baby
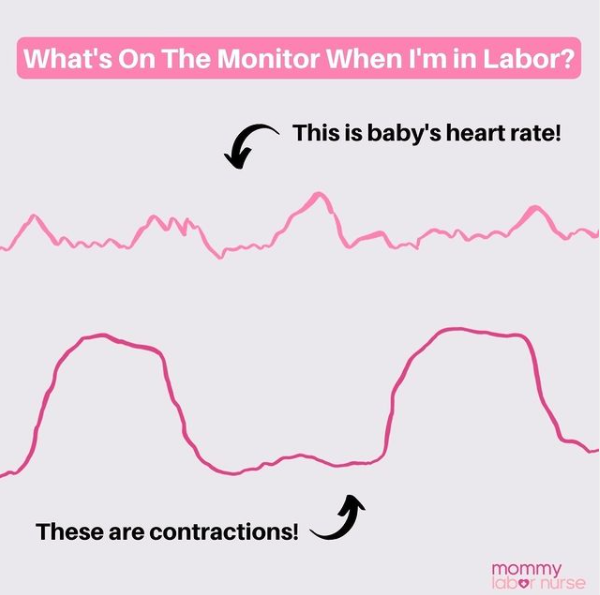
Once you’ve changed, your nurse will put you on the fetal monitor. She will hook up a contraction monitor and one to track baby’s heart rate. They are both small EXTERNAL monitors that go on your belly.
Once we put these on, UNFORTUNATELY, we can’t take them off again until your baby is on the outside.
If you have to use the bathroom really fast, it’s okay to take them off briefly, but INTERMITTENT monitoring is not allowed once we start PITOCIN (or according to your hospital’s policy).
NOW, if you’re coming in for a night labor induction to PREP your cervix for labor, we typically DO NOT have to leave your monitors on all night (unless something funky is up with baby). I would start continuous monitoring in the AM with your Pitocin…just a little tid-bit to add.
Why do we need to monitor baby nonstop during labor induction?
- We need to see your contraction pattern to titrate your Pitocin
- More importantly, we need to see your baby’s heart rate for safeguarding…in case we need to jump ship. AKA, in case we need to turn down the Pitocin, turn OFF the Pitocin, or head to the operating room…
Don’t be too bummed out about continuous monitoring – MANY hospitals still allow you to move around your room, get in the shower, and walk around the unit. As long as we can trace baby’s heart rate, you can get into whatever position is most comfortable.
4. Medical history and placing the IV (if you’re starting Pitocin right away)
While your nurse is monitoring your baby, she will be going over a series of questions for our database. Just general stuff…prenatal care, what you want to do for pain, your medical history, etc.
She will then place an IV, draw preliminary labs, and start some IV fluids. Sometimes if you are coming in for a PM induction, IV fluids won’t be started until the next morning.
5. Checking in with your provider
Your provider will come to see you next and talk to you more about your labor induction. He/she will talk about the methods that will be used, the risks vs. benefits, and scan your abdomen to see where baby is lying.
We want baby to be HEAD DOWN…we don’t like inducing BOOTY-FIRST babies!
Next, your provider will check your cervix and determine which method of induction is appropriate for you.
If you’re already 3-4 centimeters dilated…you probably will skip straight to Pitocin, instead of having your cervix prepped in any sort of way (it’s already prepped itself if it’s 3-4 cm dilated!).
6. Inserting foley bulb or medication
If you need a Foley bulb or any other “prepping” medication, this is when your provider would do that part…
Once that’s done, your nurse will keep you on the monitor for a little while. After about 20 minutes, if everything looks good, you’ll get to remove the monitors and go to sleep (or rest…it’s hard to sleep in the hospital the night before you have a baby).
7. Starting Pitocin (more details below)
Alternatively, if you’ve come in for an AM induction, your nurse will get your Pitocin started after your provider checks in!
If you’re a PM labor induction, Pitocin will most likely get started in the morning…or sometimes in the middle of the night if your Foley bulb comes out early.
Starting the Pitocin
Now, Pitocin isn’t like a WHAM BAM, THANK YOU MA’AM sort of drug. I’ve already referenced earlier, Pitocin needs to be titrated to a certain level to get you into adequate labor!
What is Pitocin like?
- MOST women do not start feeling contractions AS SOON AS Pitocin is started
- Usually after about an hour, you may start to feel some cramping, followed by mild contractions
- Then you’ll feel stronger contractions that start to get closer and closer together
Like I said, usually it takes at least an hour or so to feel ANYTHING, but I’ve had ladies feel contractions in 15 minutes, while for others it can take hours. It all depends on your body!
When will they stop increasing Pitocin?
Once you’ve reached an adequate labor pattern (remember, PAINFUL CONTRACTIONS, 2-3 MINUTES APART, AND CERVICAL DILATION), your nurse will STOP turning up your Pitocin.
Then, your body will do its thing, change your cervix, and eventually you’ll have a baby!
How long will a Pitocin induction last?
Don’t be surprised if this is a LONG time from when we first started your Pitocin. If you are a first-time mom, my PM labor inductions typically don’t deliver until the FOLLOWING night…on the night shift. It takes a LONG time (usually) for your body to get the idea that it’s time to have a baby.
But don’t stress, this is NORMAL…babies can take a long time to make appearances when they are induced!
Dos and Don’ts Before Being Induced
Now that we’ve covered what a labor induction is and how to prepare for an induction, let’s wrap up with a discussion on do’s and don’ts before being induced.
Some of the do’s and don’ts are more obvious than others, but for many mamas, this is their first rodeo, so I don’t want to assume anything.
The day before your labor induction will probably be filled with all kinds of emotions. If you are a type-A planner person then you are probably enjoying the fact that you know (for the most part) when baby is going to arrive and can make appropriate arrangements and plans.
I actually ended up going into labor spontaneously with both of my boys so never personally experienced an induction, but either way, you can expect to experience the full gamut of emotions as you near your due date, induction, and eviction day.
Here’s what we’ll cover
Let’s save the emotional discussion for another day (and another blog article). Now I want to dive into the do’s and don’ts before being induced so you will be super prepared for the big day!
We are going to start by talking about the things you should do before being induced. I touched on it some above, but depending on whether you are a first-time mama or 2nd+ time mama and how ready your cervix is, you will either start your induction in the morning (cervix is > 3-4 cms) or evening (cervix is < 3-4 cms).
This list is intended for low-risk mamas with uncomplicated pregnancies and scheduled inductions. Should a situation present in pregnancy that requires you to unexpectedly be induced, be sure to double-check with your provider before doing (or not doing) some of the things discussed below (more to come on this below)!
Things to do before your induction:
1. Eat
If you are coming in for a scheduled, routine induction, I highly encourage you to eat something before you come to the hospital.
There is a good chance that once your induction process really gets going you either won’t be allowed to eat or will be limited to clear liquid items. Policies surrounding eating during labor vary from place to place so don’t hold me to this, but where I work, this is typically the norm.
And regardless of what the hospital’s policy is about this, a lot of women experience nausea at some point during labor, so there’s a good chance you won’t feel like eating even if you can.
To go along with the whole “a lot of women experience nausea at some point during labor thing”, I would avoid a big, greasy feast before heading in for your induction. There’s a chance that whatever goes down might be making an appearance later if you catch my drift, so steer clear of anything too heavy.
Note: There are other situations where they might want you to refrain from eating so err on the side of caution and always double-check.
2. Get a good sleep or rest
I know you will be feeling all the things leading up to your induction but try, try, try to get some sleep the night before or rest the day of if you are coming in at night. Start by winding down earlier than you normally would because it might take some extra time for your mind and body to relax.
I recommend putting your cell phone away. If your friends and family know you are being induced soon then they probably will be blowing your phone up. The last thing you need when you are winding down for the night is to be answering a zillion texts or to constantly hear your phone dinging.
I also recommend a warm bath or shower, meditation, listening to some relaxing music, or reading a book to help relax you and hopefully make sleep a little easier.
3. Take a bath or shower
Depending on how long your induction takes and how you are feeling after delivery, it could be several days before you shower again.
This is obviously a personal choice, but I would definitely recommend bathing before you head to the hospital.
4. Birth plan
If you have a birth plan (which I highly recommend by the way!), make sure you have a copy and review it with your support person before going to your induction.
You might have filled it out weeks prior and may or may not have had a chance to go over it with your partner, so make a point to do this so that everything is fresh on both of your minds.
And if you don’t know where to start, I have a whole article that talks all about how to create a birth plan. The article includes a link to my free birth plan template too.
Related Reading: How to Make a Birth Plan: An L&D Nurse’s Guide
5. Date night
I recommend mamas try and sneak one last date night in with their partner the night before their induction.
I know, I know, this isn’t doomsday, there will definitely be time for date nights again at some point, but it could be a little while before you find your new groove, so take advantage of it.
Plus, it might distract you and help calm your nerves a little bit so it’s a win-win in my book!
6. Hospital bag packed
I highly recommend having the majority of your hospital bag packed by 35/36 weeks so that you are ready to go if baby decides to surprise you.
I know, however, there are a few items that you can’t pack until the last minute – and I have a tip for you to make sure you don’t leave anything behind. Put a sticky note on your bag for last-minute items!
View this post on Instagram
You will have a million things running through your head the morning or day of your induction, and the last thing you want to do is try and remember all of those last-minute items. Have those sticky notes filled out, on your bag, and ready to go!
For more tips and tricks about packing your hospital bag, including what to include for labor, postpartum, and baby, be sure to read my article below.
Related Reading: Hospital Bag Must-Haves from an L&D Nurse
Things not to do before your induction:
1. Get the party started early
I’m sure you’ve heard of all the tips and tricks to try and naturally induce labor. If you are planning on a scheduled induction there’s really no need to give these things a whirl.
Maybe you are having a post-dates (past your due date) induction and have already tried all the things with no such luck, and maybe you haven’t.
Either way, with an induction on the very near horizon, it’s probably best to hold off and let your induction do its thing. Before you know it, you will be holding your sweet baby in your arms.
2. Be afraid to ask questions & advocate
Remember, this is your journey, your birth, and your day. Don’t be afraid to ask questions, to speak up, to advocate for yourself and your baby. It doesn’t matter if this is your first baby or your fifth, each experience is unique and different!
I highly encourage you to speak up if and when questions arise. I know that for some advocating can be awkward and uncomfortable. If you can identify with this, you will absolutely want to read my article below.
Related Reading: 23 Important Ways to Advocate for Yourself During Birth and Pregnancy
3. Eat a big, greasy meal
I touched on this earlier in the dos list when I mentioned that you should eat before heading into your induction. It’s not uncommon for mamas to experience nausea and/or vomiting at some point in the labor process.
The two scenarios where I most commonly see laboring women experience nausea are after an epidural placement and in transitional labor (7-10 cm).
High-fat, greasy foods can be harder for your body to digest. I can guarantee that you don’t want to be throwing up a cheeseburger and french fries during labor, or ever for that matter. Stick to something light but filling, something with some substance, something that will “stick to your bones”.
Those are your dos and don’ts before being induced!
So, there you have it! These are the big “dos and don’ts” before being induced. One thing you might be wondering is whether or not you should take any daily medications before you report to the hospital for your induction.
Some women are on medication for blood pressure or diabetes during pregnancy. For this question, I recommend running any and all medications by your OB provider in advance and letting them tell you which ones they want you to take and which to skip the day of your induction.
And if there’s any doubt about something, run it by your OB provider. They are most familiar with your pregnancy and medical history and are the best to answer and navigate specific situations with you.
How else can I prepare for labor induction?
That’s pretty much a labor induction in a nutshell! But really, there’s a lot more you can learn to erase the unknown and get yourself feeling super confident!
Our online birth classes include an entire lesson with more details + will prepare you for the ins and outs of your labor and delivery once you are induced, too.