Whenever I talk about postpartum recovery, I get a TON of questions related to C-section recovery. So often, postpartum content focuses on recovery from a vaginal birth, but C-section recovery often has more specific and almost nuanced questions related to it.
So, in this article I’m focusing totally on C-section recovery FAQs. These are some of the questions I get most often, and a lot of them are the ones that aren’t addressed as frequently.
My hope is that this article will help the mamas with C-sections on the horizon have a better idea of what to expect, and the mamas currently recovering from their C-section will get answers to their questions all in one spot.
So without further ado, let’s jump right in!
- FAQs surrounding your C-section recovery
- Sex after C-section: What’s the deal?
- Why do I have swollen feet after a C-section?
- What should I know about incision types and C-section scars?
- When can I take a bath after my C-section?
- Is diarrhea after a C-section normal?
- Why do I have back pain after my C-section?
- What should I know about exercise after my C-section?
- Can I do skin-to-skin after my C-section?
- Should I use a belly binder after my C-section?
- Will I have gas pains after my C-section?
- What’s the best position to sleep after a C-section?
- Pooping after your C-section: What to expect?
- Tips for breastfeeding after a C-section
- Any other red flags to be aware of after my C-section?
- Looking for more info in addition to these C-section recovery FAQs?
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
FAQs surrounding your C-section recovery
Sex after C-section: What’s the deal?
The most common recommendation for sex after C-section is to wait until you are 6 weeks postpartum. Most often, your provider will clear you for sex at your 6-week check-up.
This is because even though you didn’t give birth vaginally, you’ll still experience postpartum bleeding, general soreness, and exhaustion following your C-section birth.
I think it’s also important to keep in mind that even when you’re cleared for sex at that 6-week check-up, you still might not feel physically or emotionally ready for sex yet. And that is totally normal!
Keep an open channel of communication with your partner about your feelings of readiness surrounding sex with your partner. Also, remember that there are others ways you can find connection and intimacy with them until you are feeling ready.
Why do I have swollen feet after a C-section?
Swelling after your C-section birth is very common, especially in the feet and ankles! This happens for three reasons:
- The increased blood volume during pregnancy
- The IV fluids you had during your procedure
- And the dramatic hormone shift after delivery
Basically, all of those extra fluids take some time to be redistributed and flushed out of the body. And the hormone shift can make everything a little more dramatic. But for most mamas, this pronounced swelling usually only sticks around for the first 5-10 days after their delivery.
How to treat swollen feet after a C-section
But just because it’s common, doesn’t mean it’s less frustrating! To help combat your swollen feet after C-section here are some things you can try:
- Avoid standing for too long as it can make the swelling more significant (though you’re probably not doing a ton of prolonged standing post C-section anyway!)
- Take frequent breaks from standing, and while resting or lying prop your feet up to increase circulation and flow in the lower extremities
- When you are sitting, try to remember to not cross your legs, this will restrict blood flow to your feet
- Wear comfortable shoes that aren’t too tight on your feet. Wear clothing that is loose around the ankles to avoid restricting circulation. Consider using compression stockings to help increase blood flow to your legs
- Drink lots of water to help flush out your system
When is swelling after a C-section NOT normal?
Most of the time, postpartum swelling is not a cause for concern and will go away on its own. But sometimes postpartum swelling can be a sign of a more serious, underlying condition so it is important to know when you might need to notify your provider.
Let’s take a look at the red flags:
- Swelling that you notice to be increasing instead of decreasing
- Sudden swelling that comes on quickly
- Swelling that is more significant in one leg than the other
- When pressing on the swelling you notice an indentation that lingers or persists once the pressure is released This is known as pitting edema
- Pain or irritation in addition to swelling
- Signs of preeclampsia in addition to the swelling
- Severe, unrelieved headaches
- Blurry vision
- Sensitivity to light
- Swelling of your C-section scar that is accompanied by bleeding, foul smelling drainage, or increased pain
Again, if you have any of these symptoms or any concern about swelling after your C-section, be sure to call your doctor and check in.
What should I know about incision types and C-section scars?
Okay, I could probably write an entire article dedicated to C-section incisions and scars, but I do want to touch on the topic in this list of FAQs because it really does come up so often.
So basically there are two different types of incisions used during C-sections to get to your uterus. Let’s review these so that you can understand what your scar will look like:
- Horizontal incisions: These are the most common type and they are very low on the abdomen. They tend to be less painful and less visible after healing
- Vertical incisions: These are also known as classic cuts, but they are FAR less common now and are almost never used unless there is an emergent situation where we need to get baby out fast. This incision runs from your belly button to your pubic line and tends to leave a more visible scar
Then there’s the actual uterine incision, which could be one of three options:
- Low transverse: Again, this is the most common type of incision and is used near exclusively in planned, non-emergent C-sections because it heals better and carries the least risk of complications
- Classical: This is not common at all except in some emergent situations where the classical incision is used to get to the uterus
- Low vertical: This is also not common and is very similar to the classical incision but it’s done in the lower uterine segment. It’s a little less dangerous than the classical option but is generally only used in emergencies
Understanding your type of incision is so important to help you care for it properly, but even more so for when you plan future births. This is because certain types of incisions can put you at higher risk for complications in future births.
In our online birth course JUST for C-section mamas, Birth It Up: The C-Section Series, I go into WAY more details about incisions, scars, incision care, and red flags.
Be sure to check it out if you have an upcoming C-section birth!
When can I take a bath after my C-section?
This is a question that comes up a lot, because there is literally nothing like a good soak in the tub to ease sore muscles. However, you really do need to wait a while before you can submerge your incision after your C-section.
This is because submerging your incision into non-sterile water can put you at a higher risk for infection, and it’s simply not worth the risk! Showers are considered fine as soon as mom is feeling stable and ready to shower independently. But for a bath you need to wait until your incision is healed.
It’s hard to put a hard and fast timeline on when you can take a tub because healing is different for every mama, but typically it is safe sometime between 3-4 weeks postpartum. Like with all things, the best course of action is to check in with your provider.
Is diarrhea after a C-section normal?
So, in general, acute diarrhea after a C-section is probably not cause for concern – although it is worth a call to your provider just so that they’re aware of it and can ask some follow up questions to rule out lingering issues.
But in general, diarrhea is a side effect of abdominal surgery, and that alone could be the reason you’re experiencing diarrhea. If you’re on an antibiotic post C-section for any reason, that could be causing diarrhea, too.
Lastly, if you did experience contractions there’s the possibility that stretching or other damage to your rectal muscles/pelvic floor may have occurred which can result in diarrhea.
In short, yes diarrhea CAN be normal, but this is definitely one to call about just to be safe.
Why do I have back pain after my C-section?
A number of women experience back pain after their C-section, and just know that this is very normal! It’s actually a symptom mamas experience no matter how they gave birth.
This is because your abdominal muscles have been strained, and your general alignment has been off for the past 9 months! That combined with shifting hormones that loosened your joints and muscles In preparation for birth can really cause a lot of pain.
What’s more, caring for your baby requires a lot of hunching with a curved spine if you’re not extra aware which can contribute to the discomfort.
Lastly, C-section mamas may have back pain at the site of their epidural or spinal block. This typically feels like muscle spasms and can last for weeks to months post-birth (source).
What should I know about exercise after my C-section?
The biggest difference between exercise after a C-section vs. a vaginal birth is when you can start. And like so many questions on this list, it’s hard to say when that’s going to happen for you.
It will depend a lot on your core strength prior to your C-section, but also just generally on how your body responded to your C-section and what your healing process has been like.
The definite rules of thumb are:
- Your incision is completely closed and healed
- You’re no longer experiencing any pain or soreness
- You’ve gotten clearance from your OB
This often happens somewhere between 6-8 weeks postpartum, but for some mamas, it can take 12 weeks or longer. My biggest piece of advice is to trust and listen to your body and wait as long as necessary to prevent long-term damage.
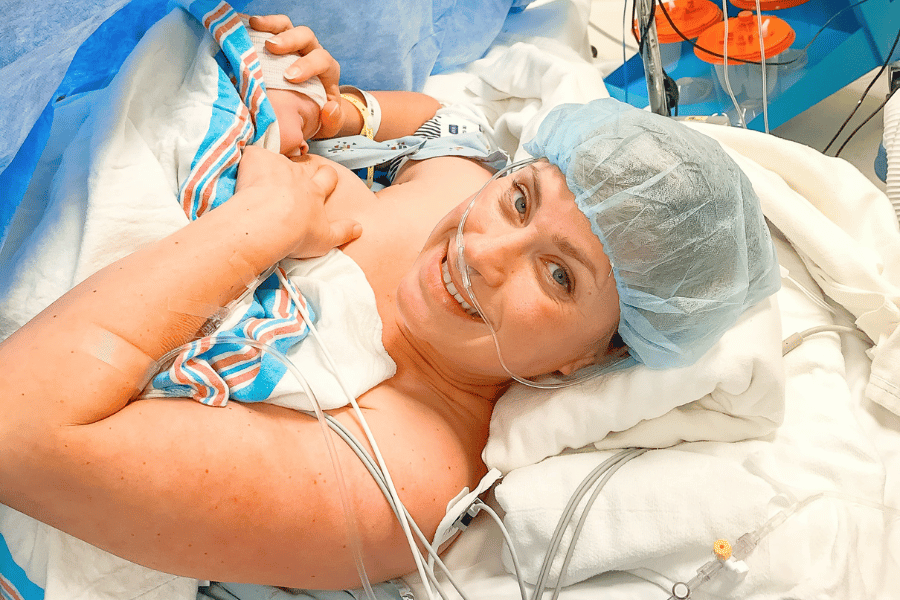
Can I do skin-to-skin after my C-section?
In many cases, yes, you can often do skin-to-skin after your C-section right in the OR! I am a big proponent for skin-to-skin after C-sections if you and baby are both stable and able because it provides so many benefits to mom and baby.
If you do wish to attempt skin-to-skin immediately after your C-section birth, be sure to indicate this on your birth plan and discuss it with your provider prior to the big day. It’s not always standard practice but can often be accommodated.
In the event that you are unable to do immediate skin-to-skin in the OR, keep in mind that your partner could stand in and do the first skin-to-skin with baby, and know that skin-to-skin benefits aren’t exclusive to the first hour after birth! Practicing skin-to-skin as soon as it’s safe for mom and baby is still beneficial.
Should I use a belly binder after my C-section?
Belly binders (also known as postpartum compression garments) can be a super helpful tool after your C-section. They provide protection for your incision, and also support the muscles in your core and back, as well as improve your posture while you are healing.
Overall, they promote general comfort as you heal after major abdominal surgery, and in some cases might even help to close the gap between your abdominal muscles if you experienced diastasis recti.
Using a belly binder after your C-section
It’s important to get the right positioning of your belly binder. You want it positioned across your hips and waist, so that it’s supporting the muscles of that low abdomen area. It shouldn’t be up high where it’s reaching your bra line.
Note that you should not sleep in your belly binder – breaks are important so don’t use it when you don’t need the support (ie: when you’re not mobile). You can read a bit more about these in this article.
Will I have gas pains after my C-section?
The answer is probably! You see gas pains are a common postpartum symptom in general, and a common symptom after abdominal surgeries, so for you C-section mamas, it’s kind of a perfect storm.
And those gas pains can be pretty dang painful from what I’ve seen and heard! You may experience them in the more typical gas pain spots we think of, but the pain can also feel like pain in the ribs, upper back, and even all the way up to the shoulders! Crazy I know.
This largely happens because of slowed down bowels and organs shifting back to their normal position after birth.
To help aid with this, veteran C-section mamas over on Instagram recommend using Gas X pills. You should also drink lots of warm liquids (like lemon ginger tea) to promote regularity in your digestive system and ease gas pains.
Related Reading: C-Section Hospital Bag List from Veteran C-Section Mamas
What’s the best position to sleep after a C-section?
It can be tricky to get into a comfortable sleeping position after your C-section because any pressure on your healing wound is super uncomfortable! Also, the general pain and soreness can make sleep difficult – not to mention the extra wakings related to newborn care, too.
Basically, you want to find a way to sleep that is going to keep pressure off your abdomen. In the first few days, this almost certainly means sleeping on your back. Some women find back sleeping more comfortable if they elevate their legs slightly with a rolled blanket or pillow under their knees. Or you can try propping up your upper body for a sort of reclined back-sleeping position.
Once your incision isn’t as sore, you can transition to side sleeping. The advantage of this position is that it may be easier to get in and out of bed without support (source).
Pooping after your C-section: What to expect?
So we did touch on the topic of diarrhea after C-section, but more often the issue with pooping after C-section is constipation-related. Your bowels often slow down significantly during birth (and during abdominal surgery in general), so constipation after a C-section is very common.
In fact, many women don’t poop during their C-section hospital stay. Often, we just want to know that at least you are passing some gas and that things are starting to get moving.
Some things you can do to help with poop and constipation after your C-section are:
- Take a stool softener regularly
- Drink warm liquids to promote regularity
- Get up and moving around frequently to help aid digestion
- When you are able and it feels comfortable, sleeping on your left side can help get things moving
Tips for breastfeeding after a C-section
Breastfeeding after birth is something that involves a learning curve for most mamas, and education about milk supply, latch, and positioning ahead of time can make a big difference! So in this list of C-section recovery FAQs, I knew I wanted to include a bit about breastfeeding as a C-section mama.
It’s ideal to start breastfeeding as soon as possible after your C-section to trigger lactation. It’s also associated with better breastfeeding outcomes. If you and your baby are stable you can often breastfeed right away (with support) in the OR, or at least within 2 hours of birth when you are in the PACU after your C-section.
If for some reason you aren’t able to breastfeed baby within 12 hours of birth (due to either of your needs), you’ll definitely want to start pumping and extracting colostrum to feed to baby and trigger your body to start making more milk.
Additionally, let’s talk about breastfeeding positions for C-section moms
- The football hold is a great position for all newborns, but with the support of a breastfeeding pillow, this can be especially good for keeping baby off of your incision
- The side-lying position ensures that there is no pressure on your incision, but keep in mind that it can be trickier to get a good latch in the side-lying position as you and baby are learning how to breastfeed
- The cradle hold also works with a breastfeeding pillow to provide protection to the incision site
Above all, I HIGHLY encourage you to utilize the heck out of the lactation consultants on staff during your hospital stay after your C-section. They can help so much with baby’s latch and positioning advice to set you up for success with breastfeeding while you are healing.
Related Reading: Preparing to Breastfeed before You Start
Any other red flags to be aware of after my C-section?
Before you are discharged from the hospital after your C-section, your provider and postpartum nurse will go over red flags and reasons to call them.
Generally speaking, any sign of infection, and anything that seems abnormal in your mind is worth a call! We’d rather you call and it be a false alarm than have something go unreported.
Here’s a brief list of things to look out for
- Swelling or redness around your incision site
- Severe pain or soreness around your incision site
- Drainage from your incision site, especially if it’s thick and yellow, green, or brown in color. Or if it has a strong, foul odor
- Fever over 100.4 degrees Fahrenheit, chills, or muscle aches
- Severe abdominal pain
- Painful urination
- Soaking through more than one pad per hour, and/or passing blood clots larger than a golf ball
- Signs of postpartum preeclampsia including increased swelling, blurry vision, and/or severe headache
- Signs or symptoms of PPD, PPA, or other postpartum mood disorders
Looking for more info in addition to these C-section recovery FAQs?
In conclusion, let me just remind you that this is not an exhaustive list but a great starting point for C-section recovery FAQs. Above all you should always follow your provider’s advice for your unique recovery!
If you’re currently preparing for your upcoming C-section, here are some other resources from MLN to help you learn as much as possible: