When it comes right down to it guys, we’ve all heard of diabetes. If you’ve been pregnant, you’ve probably talked plenty about Gestational Diabetes, even. But what is gestational diabetes mellitus, really?
Let’s talk through it a little so you have all the info you need. Maybe you’ve recently tested positive for GD. Or maybe you’re reading up on it before you’re upcoming GD test.
Whatever the case may be, I want to make sure you’ve got all the facts. I put together this guide to answer all your questions in a way that’s easy to understand. Let’s go!
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
Overview of Gestational Diabetes Mellitus
If you haven’t, mama, you’ll hear about it plenty. Gestational diabetes screenings are a part of standard prenatal care here in the US. So learning about what it’s all about will help you stay more informed.
What is Gestational Diabetes Mellitus
It’s a condition where a pregnant lady develops diabetes during pregnancy. Like, you’ve never been diabetic before and suddenly—BAM, you’ve got the ‘betes.
Diabetes is a condition where your body can’t metabolize the glucose (sugar) in your bloodstream because you can’t make enough insulin (or can’t use it correctly).
Is Gestational Diabetes Mellitus the same thing as Gestational Diabetes?
This might seem like a silly questions – but I actually hear it all the time! And yep it is!
“Gestational Diabetes Mellitus” is the official name but usually we don’t include the mellitus when speaking of it. We either abbreviate it to GDM or say gestational diabetes.
And there are actually two types of Gestational diabetes:
- A1 which is diet-controlled
- A2 which is medication-controlled
So if I’m talking about a patient I would say “The patient has A1 GDM”. Make sense?
Symptoms of Gestational Diabetes Mellitus
Gestational diabetes can be hard to spot because the most common symptoms of gestational diabetes mellitus are thirst, hunger, and excessive peeing. These are all things that happen to be common in most pregnancies without diabetes factoring into it.
Especially once your baby is sitting on your bladder. What you need to pay attention to is changes in these things.
If you tend to pee six times a day and twice at night, that may very well be totally regular. But if all of a sudden you need to go TEN times a day and once an hour at night, well. THAT might well mean it’s time to chat with your care provider.
Why Does Gestational Diabetes Happen?
In short, GDM happens because the hormones active in your body while pregnant can:
- Prevent you from making enough insulin
- Make your body resistant to the effects of that insulin
It always seems to be those pesky hormones, am I right?
Related Reading: How to Get Rid of Hemorrhoids Fast!
How Is Gestational Diabetes Mellitus Detected?
We mentioned that the first red flag as to whether or not you have gestational diabetes is if you encounter significant shifts in your appetite, mood, and frequency of urination.
This will help you personally spot the chance that you have developed gestational diabetes.
Your provider, however, has a much more powerful way of determining if you have GDM. You may have heard of it. You may have heard HORROR stories about it.
It is, of course, the one-hour glucose test. Dah-dah-DAH!
Gestational Diabetes Diagnosis
Here in US, most women are screened for gestational diabetes at about 26-28 weeks. And this is done with the 1-hour glucose test.!
You basically consume 50g of glucose in a few minutes, then get your blood drawn 1 HR later. Your provider wants to see if your body can metabolize the sugar in a certain amount of time. If your level is too high, it means your body is struggling a bit to metabolize sugar, and you may have gestational diabetes.
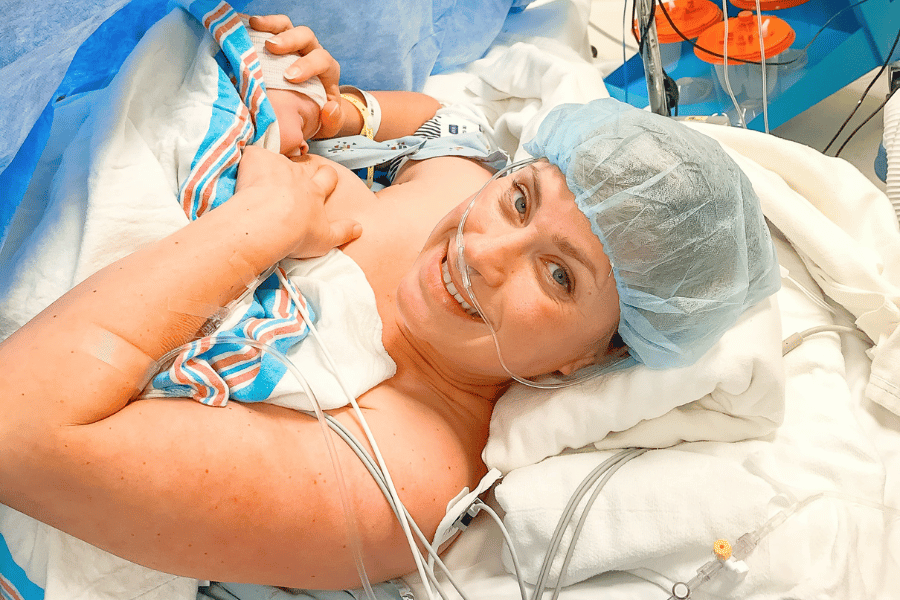
Well guess what, I FAILED my 1 HR test (only by a lil bit) so my provider recommended that I be more closely tested with the….3 HR test!
3 Hour Glucose Test

This test is a bit more accurate, but it does involve drinking another bottle of glucose (100g this time vs 50g) & you waiting around for 3 HRs & getting your blood drawn 3 times.
- When I first arrived, I had been fasting since midnight the night before, and my appointment was at 8 am
- The nurse checked a fasting blood sugar (a fingerstick), and gave me the 100g solution to drink
- I had to drink this within 5 minutes (I think it was 6-8 oz). It was a LIL nastier than the 50g solution from my 1 HR test…but not TOO bad
- Once I finished, I waited for the first hour in my car – came back to the lab & she drew my blood for the first reading. It was pretty important that I was there ON TIME, to get my blood drawn ON the hour (this can cause false results)
- After that first blood draw, I did the SAME thing two more times. Each time returning on the hour to get my blood drawn
- Once I was finished, I drove home and was able to eat again!
I didn’t have any symptoms (dizziness/nausea etc) while I was at the testing center, but oddly enough AFTER I ate some lunch that day I didn’t feel so well. But it quickly passed.
The next day my provider looked over my results and I ended up passing! Yay! All three of my blood draws were within normal limits, so I did NOT get diagnosed with GDM.
If I had failed, then I would have gotten diagnosed, followed up with a dietician & started making dietary changes in my diet along with beginning to routinely check my glucose levels throughout the day.
What happens if you have GDM?
Gestational diabetes mellitus can put you at risk for significant complications, which is why there is so much emphasis on spotting it around the 24-28 week range.
If you have GDM, your care provider will give you options. The condition is very treatable, as long as you are aware that you have it.
Monitoring Gestational Diabetes Mellitus During Pregnancy
If your doctor determines that you are suffering from gestational diabetes mellitus, they’ll provide you with the best direction on how to monitor your condition.
How aggressive you have to be with it is going to depend on severity. Your doctor may prescribe medication or insulin or might simply recommend a bit of healthy eating and some gentle exercise.
Diet Options to Mitigate Gestational Diabetes Mellitus (A1 GDM)
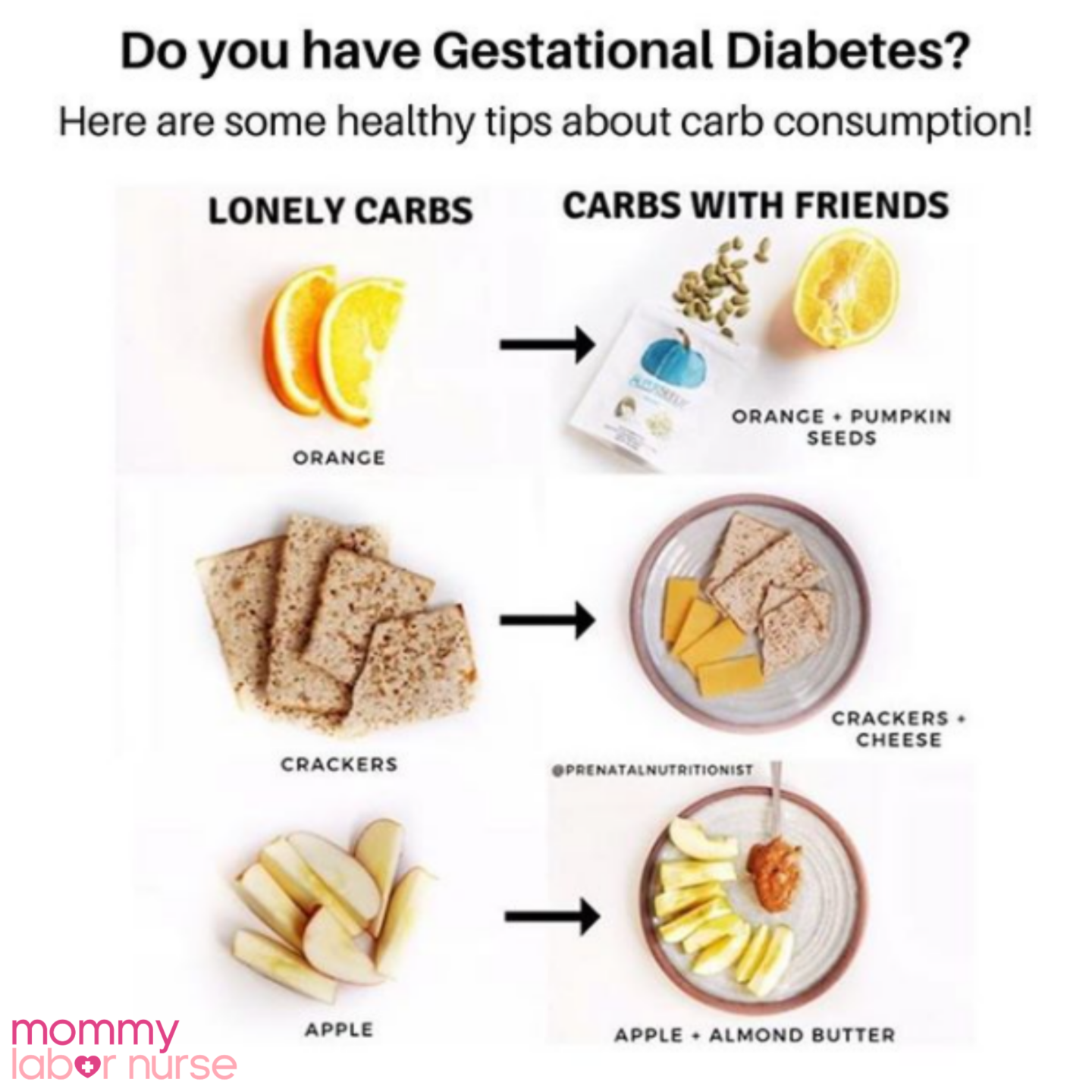
There are a lot of resources out there for how to supplement your diet with foods that help limit the impact of diabetes. Gestational diabetes is no exception.
According to the National Institute of Health, it’s important to include a wide variety of healthy foods from all groups.
Work with your care provider to establish a good, balanced plan.
Your diet should INCLUDE a substantial amount of whole grains, oils that are liquid at room temperature, and should EXCLUDE or at least LIMIT sweets, fried foods, and added sugars.
Related Reading: Pregnancy Nutrition Unpacked (Including Info for GD!)
Medications for Controlling Gestational Diabetes Mellitus (A2 GDM)
Sometimes eating might not be enough to manage gestational diabetes mellitus. Your doctor will always know best, and if they think insulin shots are necessary, definitely take their word for it.
Insulin is given as a small shot that can usually be done at home. Be sure to ask lots of questions and be straight forward about your hesitation if needles make you nervous.
Sometimes a doctor will order a prescription that can aid in the development and use of insulin inside the body, such a metformin or glyburide.
Your doctor will decide whether or not these medications are necessary for your treatment. They can be used instead of or alongside insulin.
An In-depth Look: What is Gestational Diabetes?
Now that we have a good idea of the basics, we can take a closer look at the details behind this condition.
Once you’ve taken your one-hour glucose test, ask your doctor about your target blood sugar levels during pregnancy, and how they compare to your results.
Typically a blood sugar level of over 200 while pregnant indicates excessive glucose, so that’s usually the mark you can expect your provider to be watching for.
Symptoms of Gestational Diabetes Mellitus
As mentioned above, there are a few common concerns that can indicate your blood sugar might be high. Unfortunately, even these can be pretty subtle or entirely absent in a case of gestational diabetes mellitus.
The truth is that the only surefire way to find out is to take a test.
Luckily, your care provider knows what to watch for and the timing of the glucose test is certainly no accident—it is the right time and the right conditions to find out how you are managing your insulin before development issues can crop up.
Per the American Diabetes Association, here are a few common symptoms that might indicate you have diabetes:
- Frequent urination
- Thirst or hunger
- Fatigue
- Slow healing
- Blurred vision
- Loss of weight without significant change in eating or exercise habits
- Tingling or numbness in extremities (hands and feet)
Causes of Gestational Diabetes Mellitus
What causes Gestational Diabetes? We talked a little about the why, but as a reminder, GDM is caused by an inability to create or make use of enough insulin to pack glucose into your cells.
Insulin is necessary to move glucose (blood sugar) into the cell to be used as fuel. When you are pregnant, growth and stress hormones can limit your supply of insulin and make it more difficult for the insulin to move the glucose.
Risk Factors Involving Gestational Diabetes Mellitus
Gestational diabetes risk factors can include (but are not limited to):
- Pregnancy in women older than 35 years of age
- Obesity (greater than 25 BMI)
- Excessive pregnancy weight gain
- A family history of diabetes
- Being shorter than 5 feet tall
- Excessive central body fat
- Having a larger fetus
- Carrying an excess of amniotic fluid (polyhydramnios)
- Hypertension/preeclampsia
Complications of Gestational Diabetes Mellitus
GDM complications can typically be avoided by ensuring that you work with your medical staff and take their advice seriously.
Some thing that can happen if you don’t manage your gestational diabetes correctly are:
- An overfed baby, which can typically grow larger than normal—particularly their head
- The need to have a C-section (owing to the size of your unborn child)
- Preeclampsia, or high blood pressure
- Low blood sugar (hypoglycemia) for you (and your baby, after birth)
Related Podcast: Preeclampsia, Vacuum Extractions, and Inductions: Ashley’s 3 VERY Different Birth Stories!
Prevention of Gestational Diabetes Mellitus
There are all sorts of rumors and old wives’ tales out there about gestational diabetes. The reality is that these things grow from the small truths that midwives and doctors have been practicing for eons, sometimes without really knowing why.
Can stress cause gestational diabetes? Are you more prone to diabetes if you eat a lot of a certain food? Is there a genetic component?
There’s actually a lot that’s unknown.
The role of prenatal nutrition and exercise
The reality is that we can wonder about these things until we are blue in the face. But, the prevention is the same as the cure: eat well and stay active.
That said, nothing can truly rule out the potential for gestational diabetes, or complications relating to it. Sometimes the healthiest and most active among us still wind of with GD. There’s still alot unknown about it!
That said, if your BMI is over 25, you can potentially drop your chances of getting gestational diabetes mellitus by a whopping 10% (from 16% to 6% chance) just by changing your diet for the better.
Paring a little exercise with that can decrease your risk even further.
Does Gestational Diabetes Go Away?
Gestational diabetes mellitus is a temporary condition that will go away once you deliver your baby.
However, having GDM does increase your risk of having type 2 diabetes later in life.
Moving Beyond Gestational Diabetes Mellitus
Diabetes sounds scary. We all hear about it in stories and anecdotes that serve as a cautionary tale about eating well. Sugar is vital for life, but our culture has overindulged in sweets and fried products, which have become a mainstay for childhood and adulthood alike.
Don’t let this unfortunate fact detract from your pregnancy experience, guys.
Take the time to really understand your options and do what’s best for yourself and your little one by eating healthy and keeping those feet moving.
If you take the time and make the effort, that pesky worry of “what is gestational diabetes mellitus” will become a fear of the past.
Happy healthy eating, mama!