Let’s talk about gestational hypertension and preeclampsia, mama! This is a pregnancy complication that is SO important to learn about because monitoring and treatment are key.
Now you may be wondering, what even is gestational hypertension and preeclampsia? While they’re not one and the same, both are characterized by high blood pressure.
You see, gestational hypertension can turn into the more serious preeclampsia, HELLP syndrome, or eclampsia if it’s not monitored and treated properly.
Let’s take a deep breath and unpack this together. A solid understanding of gestational hypertension warning signs goes a long way in treating this condition if it does occur for you!
- Gestational hypertension (and blood pressure!) unpacked
- High blood pressure (hypertension)
- Gestational hypertension
- Screening during prenatal visits
- Warning signs of gestational hypertension
- Risk factors for gestational hypertension
- Why is gestational hypertension a concern for me and my baby?
- Gestational hypertension treatment
- What about chronic hypertension in pregnancy?
- Let’s talk about preeclampsia
- Other complications of gestational hypertension and preeclampsia
- Can gestational hypertension and/or preeclampsia be prevented?
Follow @mommy.labornurse on Instagram to join our community of over 650k for education, tips, and solidarity on all things pregnancy, birth, and postpartum!
Gestational hypertension (and blood pressure!) unpacked
High blood pressure (hypertension)
Blood pressure is the force of blood that pushes against the walls of your arteries. Arteries are blood vessels that carry blood away from your heart to other parts of the body.
High blood pressure (also called hypertension) is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy
Gestational hypertension
Gestational hypertension is defined as high blood pressure that occurs in pregnant women after 20 weeks gestation, who did not have high blood pressure prior to pregnancy. It’s usually defined by blood pressure readings above 140/90 WITHOUT the presence of elevated protein levels in their urine.
If there is excess protein, it’s more likely preeclampsia, which we’ll discuss in detail below.
Screening during prenatal visits
So, now are you thinking – that’s why my provider checks my blood pressure and urine at every single prenatal visit! It really is one of the best ways to monitor you for pregnancy complications including gestational hypertension and preeclampsia.
You see, the sooner we can catch gestational hypertension (and even preeclampsia) often the more successful we can be at treating it and monitoring baby to let them stay in there are long as possible!
Warning signs of gestational hypertension
Interestingly, gestational hypertension sometimes comes with a host of symptoms, but in a lot of cases, the ONLY symptom is a high blood pressure reading.
This is why regularly scheduled prenatal visits are so important – screening really is one of our best tools! But it CAN be accompanied by other symptoms.
Here’s a complete list of gestational hypertension symptoms
- Blood pressure reading over 140/90
- Excessive swelling and water retention (medically referred to as edema)
- Big jump in weight gain in a short time frame (this is why plotting/tracking your weight gain is important, too!)
- Changes in vision (blurriness, double vision, or floaters)
- Headache that won’t go away
- Nausea or vomiting (aside from first-trimester nausea)
- Making small amounts of urine
- Pain in the upper right side of your belly
*If you have some of these symptoms, along with protein in your urine, you may have developed the more severe condition, preeclampsia*
Risk factors for gestational hypertension
While the root cause of gestational hypertension for a lot of mamas is unknown, there do seem to be certain factors that put you at higher risk of developing gestational hypertension.
- High blood pressure prior to pregnancy
- Kidney disease prior to pregnancy
- Family history of gestational hypertension
- History of gestational hypertension
- Diabetes
- Pregnancy in women younger than 20
- Pregnancy in women older than 40
- Pregnancy in black women
- Pregnant with multiples
Why is gestational hypertension a concern for me and my baby?
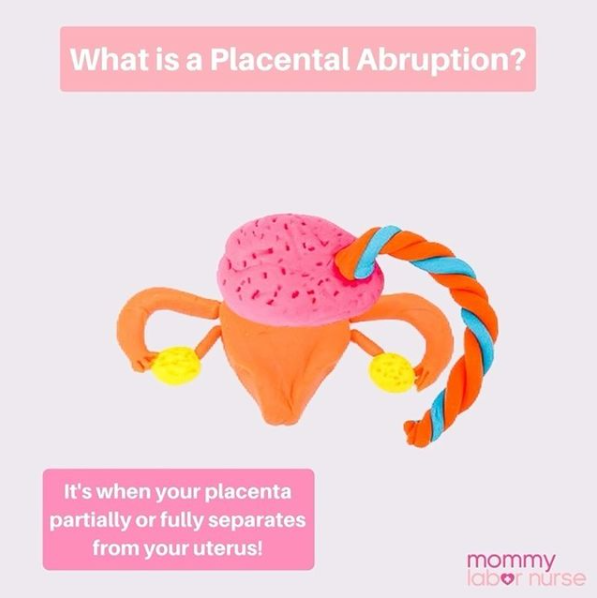
The main concern with gestational hypertension is that it will develop into preeclampsia – which has much more serious effects (such as seizures, placental abruption, and stillbirth).
However, gestational hypertension carries risks on its own because when your blood pressure is high it affects your blood vessels.
- May stress your organ system function due to decreased blood flow
- Can result in decreased blood flow to your placenta which in turn means fewer nutrients and oxygen for baby
- It may be associated with low birth weight or poor fetal growth (as a result of placental problems)
- Can lead to preeclampsia
Gestational hypertension treatment
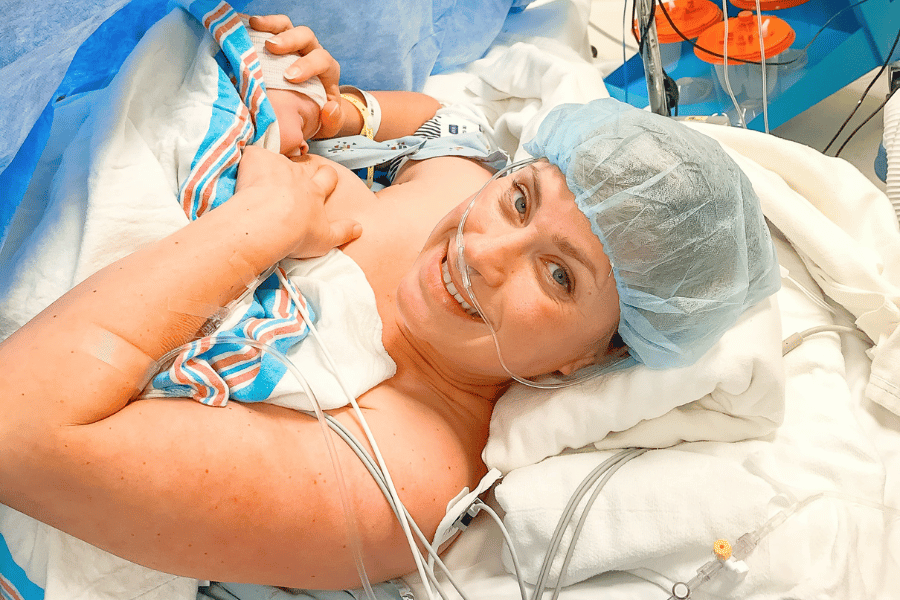
The best treatment for gestational hypertension is usually delivery! Often, providers will try to get you to 37 weeks and then schedule an induction of labor to ensure the safety of mom and baby.
But of course, if you haven’t reached a point in pregnancy that is safe for delivery, other measures will be taken.
These treatments involve increased monitoring of baby, attempts to lower your blood pressure, decreasing the risk of your blood pressure rising higher, preventing more serious complications from developing, and preventing preterm delivery.
Here are the usual treatments:
- Bedrest: This is a very common form of treatment, but actually research only shows it to be mildly effective at decreasing the risk of increasing blood pressure and preterm labor. Sometimes, and in severe cases, you may be kept in the hospital
- Blood pressure medication: Medication is an effective form of treatment, but is used with caution because medication can put baby and mama at risk for other issues. Typically, medication is used only if blood pressure is very high, or delivery is far away
- Dietary changes: Again, there isn’t a TON of research that supports this, but most providers will recommend dietary changes that aim at lowering blood pressure. This includes lowering your salt intake, filling up on more lean protein, and staying well hydrated!
- Increased prenatal appointments: This is the big one that will be true for ALL women with hypertension disorders in pregnancy. Your provider will want to see you weekly to monitor your blood pressure, urine protein, and other symptoms, additionally they will increase monitoring for baby
- Increased fetal monitoring: Often your increased prenatal appointments are accompanied by weekly ultrasounds to monitor baby’s growth and development, and make sure the placenta is doing its job
- Non-stress tests: This is a test that measures baby’s heart rate in response to fetal movement
- Kick counting: This is good practice for all pregnant women, but will be especially important and recommended if you have high blood pressure during pregnancy
What about chronic hypertension in pregnancy?
Chronic hypertension is similar, but it’s defined as high blood pressure that emerges before 20 weeks gestation OR prior to pregnancy entirely.
Chronic hypertension will be monitored and treated similarly to gestational hypertension, and carries the same risk factors to mama and baby, and the potential for more serious complications to develop.
Let’s talk about preeclampsia
OKAY. So if you made it here, you already heard me refer to preeclampsia quite a bit. This is the (often) more serious form of gestational hypertension because it’s associated with greater risks to you and baby.
Preeclampsia is a condition that occurs after 20 weeks gestation (and even into postpartum!) mainly characterized by high blood pressure AND excess protein in your urine.
This excess protein indicates that there are issues going on with your organ systems (usually the kidneys or liver).
How common is it?
Preeclampsia is a serious health problem for pregnant women around the world. It affects 2 to 8 percent of pregnancies worldwide (2 to 8 in 100).
In the United States, it’s the cause of 15 percent (about 3 in 20) of premature births. Prematurity is birth that happens too early, before 37 weeks of pregnancy.
Awareness is so important!
Many women do not know what pre-eclampsia is, but it can be very dangerous, and one of the MAIN reasons mamas get induced early or have emergency C-sections.
Fortunately, with frequent screenings and when it’s caught early, most women with preeclampsia have healthy babies. But it it’s left untreated; it can cause severe health problems for you and your baby.
Preeclampsia vs gestational hypertension
The main difference between preeclampsia and gestational hypertension are signals that mama’s organs are already being affected by the high blood pressure.
This is usually indicated by elevated protein levels, blood platelet counts, and other tests that check liver and kidney function.
Most often preeclampsia develops in the third trimester AFTER week 34 of pregnancy. When preeclampsia occurs before then, it’s referred to as early-onset preeclampsia.
Early-onset preeclampsia can be more challenging because it’s important to keep you safe while giving baby the most time to develop as possible!
In rare cases, it can even develop AFTER birth, and is then referred to as postpartum preeclampsia.
Warning signs and symptoms of preeclampsia
The warning signs are similar to gestational hypertension, with added symptoms that indicate a more severe condition. The complete list of symptoms includes:
- Swelling of face and hands
- Headache that won’t go away
- Blurry vision, seeing spots, changes in eyesight
- Pain the upper right side of your belly
- Shoulder pain
- Unexplained, sudden weight gain
- Difficulty breathing
- Low number of platelets in blood
- Fluid in lungs
- Severe headaches
- Abnormal kidney or liver function
- Systolic pressure of 160 mm Hg or higher or diastolic pressure of 110 mm Hg or higher
Symptom information obtained from the American College of Obstetricians and Gynecologists
Risk factors for preeclampsia
- High blood pressure prior to pregnancy
- Kidney disease prior to pregnancy
- Past pregnancy with preeclampsia
- Family history of preeclampsia
- Diabetes
- Autoimmune conditions (such as lupus)
- Pregnancy in women older than 35
- Pregnancy in black women
- Pregnant with multiples
- Close interval pregnancy
- IVF conception
- Obesity
Risk factor information obtained from The Mayo Clinic
Dangers and complications of preeclampsia
Preeclampsia is a serious pregnancy condition because of its potential to cause harm to you and baby. Here are some of the complications associated with preeclampsia:
- Fetal growth restriction due to issues with the placenta
- Necessity of preterm delivery, which puts baby at risk for a variety of conditions associated with premature birth
- Placental abruption
- Eclampsia (more below)
- HELLP syndrome (more below)
- Organ damage
- Cardiovascular disease
Preeclampsia treatment
Treatment for preeclampsia is largely the same as the detailed treatments discussed in the gestational hypertension section.
Largely your provider will monitor baby more closely and frequently, will likely put you on bedrest and/or blood pressure medication, and you will very likely be induced at 37 weeks.
In some cases, when preeclampsia is severe or progresses to eclampsia or HELLP syndrome, you may be induced even earlier.
This will be a discussion with your provider wherein the risks of preterm delivery are weighed against the risks to you and your baby’s health by remaining pregnant.
Other complications of gestational hypertension and preeclampsia
HELLP Syndrome
HELLP syndrome is a life-threatening pregnancy complication usually considered to be a variant of preeclampsia (very rarely does it appear in the absence of preeclampsia). HELLP syndrome is rare, affecting 1-2 women per 1000 pregnancies.
HELLP is an acronym that stands for:
- H – Hemolysis, which is the breaking down of red blood cells
- EL – Elevated liver enzymes
- LP – Low platelet count
HELLP syndrome can be difficult to diagnose, especially when high BP and protein in the urine aren’t present. Its symptoms are sometimes mistaken for gastritis, flu, acute hepatitis, gall bladder disease, or other conditions.
Symptoms and treatment for HELLP syndrome
It’s super critical for pregnant moms to be aware of the condition and its symptoms so they can receive early diagnosis and treatment! The symptoms of HELLP, outside of tests done on platelet levels, red blood cells and liver enzymes are the same as the symptoms of preeclampsia.
- Most often, the definitive treatment for HELLP Syndrome is the delivery of baby (similarly to the treatment of preeclampsia!).
- Many women suffering from HELLP syndrome require a transfusion of some form of blood products too (red cells, platelets, plasma).
Again, delivery is the number one treatment for HELLP syndrome and the timing will be assessed based upon your week of gestation and condition.
Information from the Preeclampsia Foundation
Eclampsia
Eclampsia is another rare but very serious complication of preeclampsia wherein high blood pressure leads to life threatening seizures during pregnancy. Eclampsia occurs in 1 out of every 200 women that are diagnosed with preeclampsia.
Most symptoms of eclampsia are the same as preeclampsia, with the addition of seizures, loss of consciousness, and agitation. In some cases, women do not have any notion of preeclampsia, and symptom onset begins with the extreme scenario of a seizure or passing out.
The most significant complications of eclampsia are seizures and placental abruption, in addition to premature birth and fetal growth restrictions.
Can gestational hypertension and/or preeclampsia be prevented?
Unfortunately, there’s not a lot you can do to prevent these complications from happening. BUT, here’s what you CAN do:
- Keep up with your regular prenatal visits during pregnancy
- Inform your provider about any previous high-risk pregnancies or family history of HELLP syndrome, preeclampsia, or other hypertensive disorders
- Understand the warning signs and report them to your provider immediately
- Trust your gut when “something just doesn’t feel right” – self advocate, mama!
Fortunately, with modern medicine, and doctors’ ability to track and monitor baby so well during pregnancy, outcomes are usually good for mama and baby as long as we know what we’re up against!
But please understand, that spotting this condition is SO important for you and baby’s safety.
I know many mamas in the Mommy Labor Nurse community have shared their preeclampsia, eclampsia, and HELLP syndrome stories so that others can learn.